This is Your Anxiety Toolkit - Episode 203.
Welcome back, everybody. Today’s episode is all about why it is so important that we expose ourselves to our fears. It’s one of the most common questions I get asked from my clients, right? Which is, why do I have to do this hard work? Why? Why of all the treatments is mine the one where I have to face my fears. Because my clients ask this all the time, I wondered whether you needed a quick pep talk just to get you back on track, to remind you why and to motivate you towards facing your fears, because it is probably the most valuable change of behavior that you will do.
Welcome back. I am so happy to have you here with me today to talk about that specific topic. Before we get started, I would like to quickly dive in to really set the scene today. We’re going to talk about the hard thing, the “I did a hard thing” segment.
Today’s hard thing is from anonymous, and they have submitted saying:
“I haven’t drank coffee for over two years since my OCD breakdown because I was too scared. But today, I went to Costa and I had a caramel latte. I got heart palpitations for a few hours, but I sat with it.
This is exactly what I’m talking about. So, Anonymous, this is so good. I am so proud of you. This is the work that we do. And I’m going to use Anonymous’ example here throughout the podcast to really tie this together.
All right, one more thing before we get moving, I want to do a shoutout to the review of the week. This one is from Hahajack, and they said:
“This is the best short therapy lesson. This podcast is amazing! I love that episodes are short and succinct. You can’t say that you don’t have time when episodes are as short as 10 to 30 minutes. If you are struggling with OCD or anxiety, this is a great podcast to listen to for extra therapeutic support in addition to therapy. I treat OCD and I learn so much every time I listen to Kimberley’s podcast.”
Thank you Hahajack for that amazing review. We are still doing the drive for reviews. So if you can go over to Apple podcast, leave us a review or wherever you listen. Once we hit a thousand reviews, we’re giving a free pair of Beats headphones. I cannot tell you how much I love, love, love, love your reviews. Thank you. It helps me help more people reach more people. And that’s what I’m here to do. All right, so let’s get to the meat of this episode, right?

I, in the past – I think it’s Episode 86 – did a whole episode called the Science of Exposure and Response Prevention. You can go back and listen to that episode once this is done. We talked about the science behind ERP, and I’m going to be using a lot of that reference to talk about why. Why do we stare fear in the face?
Instinctually, when we have fear – I’m just going to give you a quick education here – when we experience fear and our brain sets the signal off to say, “There might be danger, there might be trouble, please be alarmed,” – when the anxiety hits our body and our cognitions, our natural instinct is to remove ourselves from the perceived danger. And that has kept us alive. It is an important process that we humans have and other animals have. It’s an important piece that keeps us alive, like I said.
The problem is, that behavior, the removal of anxiety, the avoidance of the thing that created the anxiety is only effective if the danger is imminent, not just a thought about a possible danger, right? And so, if, like I said, there was a real thing that was happening in your life that is dangerous, yeah, you may want to remove yourself from it. But if you have a brain that’s anxious like mine, where your brain sets off alarms quite often telling you, “Ring, ring, ring, something bad might happen. Ring, ring, ring, the future may have some problems. Ring, ring, ring, you’re a bad person,” and so forth – when we instinctually try to remove that, we actually reinforce the fear, the faulty fear. We reinforce the thought, right? And then what we are in a cycle of is thought, reinforcement of thought, thought, reinforcement of thought, thought, reinforcement of thought.
The whole reason we choose to face our fear is to break that cycle, right? If you have a thought about imminent danger or threat, and you respond to it as if it’s important, your brain will continue to perceive it as an important and an imminent threat. If you have a thought about something that is imminent and dangerous, and you don’t respond to it as if it’s imminent and dangerous, your brain starts to learn not to set that alarm every time you have that thought. Your brain learns not to ring the alarm bell and send out all those anxiety hormones throughout your body. Right? And that’s how you break the cycle. And we do that by – if you just happen to have the thought, you could do that by being aware that you’re having the thought, observing the thought, and then not engaging in the avoidant or reactive behavior, right? That’s hard, right? It’s doable, but it’s hard, right? Because you have to be aware and you have to be very mindful and you have to have a lot of motivation in that moment. I still strongly encourage you to try that and practice it every single day.
But what we can do to really help that process is, instead of waiting for the thought and then practicing not just engaging in that thought as if it’s real and imminent, what you can do is purposely expose yourself and purposely bring on those thoughts by facing your fears. Right? Think of it like, you wouldn’t just show up to a football game or a tennis game or a track and field event and just run and hope that your body will keep you going. No, we don’t do that. When we know there’s an event happening, we train for it. In a situation, we simulate the scenario, right? So we simulate the track and field event, or we simulate the soccer practice so that you can practice strengthening those muscles.
This is why it’s so important that we choose to expose ourselves to our fears on purpose. You’re training your muscles to respond differently. When it does have a thought, your brain’s going, “Oh, she actually purposely had that thought yesterday. So maybe I don’t need to set off the alarm bells this time. Maybe it’s not as imminent as I originally perceived it to be.” That is why it is so important that you expose yourself to your fears.
Now, like I said, there’s lots of science behind that. You can go back and listen to the episode – it’s number 86 – to get a little bit more, right? But the thing here to remember, and I always try to remind you, is it is hard. This isn’t easy, right? So what you want to do is, as you go to face your fear and expose yourself to your fear on purpose, you want to keep in mind for yourself your own why. Why would I purposely do this hard thing?
We could use the example here of the hard thing, right? They wanted to have a caramel latte. They don’t want to feel uncomfortable, but they want the outcome. They want the delicious, warm caramel latte, right? For you, be really clear on what you want to get back by facing your fear. Sometimes it’s more time with family, it’s to be able to get to work and not have to manage mental compulsions with work. For some people, it’s to be able to get through school without having to double-check your work. For some people, if you have an eating disorder, it might be so you can be with friends and have freedom around food. If it’s panic disorder, it might be so that you can do the things you want to do without panic-making your choices, right? If it’s hair pulling and skin picking, it might be so that you can do your normal grooming without engaging in these behaviors. Right?
So there’s so many reasons why we would practice facing your fear. And I want to give you this call to action, which is, get really clear on what you want, how you want your life to be. Identify what things you’re going to need to face in order to get that life. And then go and face those fears. That’s exposure and response prevention in a nutshell. In a nutshell, and it might feel really silly. You might be thinking, oh, I’ve got to do so many steps just to be able to get out the door or go to school, or to be able to have a dinner party or even get out of bed. Okay, that’s all right. Break it down into small baby steps. For every time you face your fear, you’re strengthening that muscle of being able to tolerate discomfort.
It’s so important. It’s so empowering. It’s why I always say, it’s a beautiful day to do hard things, because it’s a total flip flop on what your natural brain wants to do, your instinctual brain, which is, it’s a beautiful day to run away from hard things. So really remember that. It is a beautiful day to do hard things. Really think about what you want to be able to do with your life. Write down what fears you’d need to face to do that, and then go and face those fears. That’s what I’m going to encourage you to do.
That being said, I, myself, am about to embark on a very, very hard thing, which is the exciting news. I’m almost done with this episode. I’m going to drop you my exciting news, which is the book, the Self-Compassion Workbook for OCD comes out literally next week. You can go to wherever you buy your books to get it. It’s called the Self-Compassion Workbook for OCD. It is literally the example of facing your fears. I have quite a large degree of anxiety about this, but I am going to face it every step of the way.
That being the case, because I am so insistent on facing my anxieties about it, sort of feels like I’m putting myself out there a lot – next week, I am going to announce an exciting, what would we say celebration of the book. It is going to be a month-long celebration. I hope you come along for the ride. In order to really benefit from this celebration, you will need to sign up for the newsletter because I will be sending tons of resources for you. I’m going to try and get you to engage in self-compassion like you have never done before. I want to use this as an opportunity to teach you and deep dive into the practice of self-compassion like you’ve never done before. You can go at your own pace. I strongly encourage you to sign up for the newsletter. You can go to cbtschool.com to sign up and it will give you tons of information. But next week’s episode, I’m going to tell you all about it, and I am so excited. So, so, so excited.
If you want a ton more information, you can go and follow me on Instagram. I’m going to be doing a ton of lives, talking about the book, reading through the book, showing you some of the exercises. I’m just so excited. I’m almost a little too excited. I’m probably going to burn out midway, but I’m going to do my best not to do that. But please do stick around. I cannot wait to share that with you. I will give you all the information next week. Yeah, so excited. And go ahead and get the book if that’s something that would be beneficial for you.
Well, that is all I have to say for today. That is the core of this podcast – facing your fears compassionately, willingly, in a joyful way. Even I encourage you to make it in any way possible, joyful. That is what I want you to do, and I’m really so excited to hear all of the hard things that you guys are doing because that’s what we’re here for. If that’s the one big impact I can make in my career, I’m going to be a happy camper.
All right. I am sending you so much love. I hope you are well. It is a beautiful day to do hard things. I love you so much. Take care of yourself and I will see you for a very exciting episode next week.The Self-Compassion Workbook for OCD is here! Check the link HERE for more information.
This week we interview Drew Linsalata, an amazing friend who has written an amazing book called, “Seven Percent Slower” Click the link below to hear more about his book!
https://theanxioustruth.com/seven-percent-slower/
Kimberley: Welcome, everybody. This episode is for you, the listener, but it’s actually for me, the podcaster, more than anything.
Today, we have the amazing Drew Linsalata. I’ve talked about Drew before. We’ve done giveaways. We’ve done a bunch of stuff together on social media. I am a massive Drew fan. So, thank you, Drew, for being here today.

Drew: Oh, you’re so sweet. Thank you, Kim. It’s my pleasure to be here.
Kimberley: Okay. So, you, you are amazing, and I would love if you would share in a minute to people a little bit about your lived experience with anxiety. Drew is just the coolest human being on the planet. So, I’m so excited to share with everybody you, because I think everybody needs Drew in their life.
Drew: Wow.
Kimberley: But in addition to that, we are today going to talk about something. I’m actually going to try and drop down into my own vulnerability, and not just be the host, but also be the listener today because you are talking about one particular topic that I need to work on. So, first of all, tell me a little bit about your background, your story, and we’ll go from there.
Drew: Sure. So, unfortunately, I lived in experience with panic disorder, agoraphobia, and intrusive thoughts and things of that nature, clinical depression, on and off, from the time I was 19 years old – 1986 all the way to around 2008, in varying degrees. So, it was a very long time. I was in and out of those problems. They came, they went. I did all the wrong things for a lot of time, trying to fix those problems, even though I knew what the right things were, because I’ve always been a bit of a behaviorism and cognition geek. And it took me a long time to come around to actually solving those problems. I did the medication thing that didn’t work out for me. And then I really just took the time to learn what I needed to do behaviorally, cognitively, using those evidence-based things that I know you talk about all the time. And I just used them on myself and I learned as much as I could from very smart people like you. And I went and did the work and managed to get myself through the recovery from panic disorder and agoraphobia and depression and all of those things.
And along the way, the things that I learned, I just started sharing with other people, which is nothing that I invented. I never claimed that I invented any of this stuff. I just became a really good messenger, I guess, in terms of explaining. Well, I learned this and then I used it this way. And that led to just helping people online back in 2008, 2009 as I was going through it. And that led to continuing to do it. And that led to starting my own podcast back in 2014, like talking to nobody with a $4 app on my phone. But it just seemed like the right thing to do to try and pay the help forward, because I had a lot of supportive people who rallied around me. And that just one thing led to another.
And here we are, and the podcast is just kept going and it has led to writing two books about this stuff. One is my story, and one is the recovery guide that I wrote. And here I am, still educating about this topic and advocating and supporting where I can and just trying to contribute to the community because I felt like the community, in its form that it was in 10, 15 years ago, was so helpful to me. And I just feel like I want to give as much of that back as I can. So, yeah.
Kimberley: So you’ve written-- I’m giggling. So, for everyone listening, if you hear me giggling, it’s not because it’s particularly funny. It’s just so ironic to me. You wrote a book called Seven Percent Slower.
Drew: Yes.
Kimberley: Now I probably tell my clients every single day they need to slow down. I have done a podcast on slowing down, but it is probably the safety behavior I fall into the most. And I don’t do a ton of safety behaviors anymore that this one is just so ingrained in me. So, I read your book. Thank you so much. Not only is it an amazing read, but you’re hilarious. I was texting Drew yesterday, just cracking out at some of the things that he says because it’s my type of humor. I just love it. So, can you share with me why this one topic? Of all the things you could have written, why is this one topic? Why was it so important to you and why is it so important?
Drew: It’s a good question. Up until three, four months ago. I would have not thought that I would write this book. There was no plan to write a book about learning to slow down. But what I discovered was, Seven Percent Slower is the thing that I just came up with as a little silly mental device for me when I was struggling in a big way. I knew that part of what would happen when I would get really anxious and I would begin to panic, and I would just associate that with all those nasty things, I would start just really speed up. I would rush around like crazy. And I knew I was doing that, and I knew that wasn’t helping me, but I was having a hard time catching it. And one of the things that my therapist at the time, she was like, “Really, you got to start to learn to slow down.” So she gave me that good advice. Again, I didn’t invent any of this. And I used to have to remind myself, I would literally walk around trying to remind myself like, “Slow down, moron. Slow down.” I would be talking to myself. The no self-compassion there, like, “Slow down.” And I was trying and trying and trying.
And then for some reason, because I’m a fan of the absurd, the idea of trying to go 7% slower was born in like 2007 in my stupid brain. And it was just easy to remember, “Oh yeah, just go 7% slower. And it was just a little mental trick not to actually go 7% slower. Just remind me again to slow down. And it proved to be really helpful to me like that stuck in my head because it’s silly. It’s just a silly, arbitrary number. And I forgot all about it. I use it. I still use it to this day, but not really thinking of it consciously. And I have to tell so many people in the community surrounding my podcasts and my books that slow down. One of the things to do slow down – I started telling people, “Well, just try going 7% slower.” It came back to the surface again. And the response that I got from it was astounding, like, “Oh, that’s so great. Yes, I’m using it. I’m doing the 7% slower thing and it’s really helping me.” And I’m like, “Oh, there’s a book. I need to write this.” And that’s how I dragged it back up from 10, 15 years ago. And I said, “I should probably write about this and tell people what it is.”
Kimberley: So, tell me how you implemented it in-- you’ve talked and I’ve heard you talk about exposures and some of the experiences you did. Can you just give me upfront for people who, first of all, want to hear about your story, what were some of the exposures you engaged in and how did slowing down impact it, both for how did it make it easier and how did it also make it more difficult? What was your experience?
Drew: So I’ll give you a typical morning for me. My biggest issue was-- again, my official diagnosis would have been panic disorder with agoraphobia, right? So I had a real problem leaving the house or being alone by myself or going any appreciable distance from the house. And so, a typical exposure for me, a typical morning for me when I decided I really have to fix this as I would get up, the minute I open my eyes, I put my feet on the floor, I would already be in a state of very heightened state of arousal and anxiety at that point because I knew it was coming. I was going to get dressed. I was going to get ready. I was going to hurl my butt out the door and start driving, which is the thing I was terrified to do. So, I did that every day, every single day.
And right away, I learned within the first week or so like, okay, I get the principle of this, but I’m walking out the door in a blind panic. So I need to dial it back and start to work on just preparing to walk out the door first. So, I need to really acclimate to this first. And that’s when I really started using the “Slow down, slow down, slow down.” So, I would get up and I would be trying to get ready and rush around and drink water and do everything I had to do to get out the door like I was on fire and it was crazy. And I started to slow down that way. And it really was a huge help, but you’re right, it also made it worse because-- and this is so funny because it came up in a live I did the other day on Instagram with Jen Wolkin. She talks about mindful toothbrushing. And that is really-- the act of brushing my teeth in the morning is where Seven Percent Slower really began to shine.
I wrote about it in my first book. The first thing I did before I learned to drive again was to learn to brush my teeth slowly and mindfully while I was in a complete state of panic. Yes. And just the act of slowing everything down, all I have to do is take the cap off the toothpaste. All I have to do is put the paste on the brush. All I have to do is put the cap back on. All I have to do is pick up the toothbrush. I literally would have to break down my getting-ready routine into the tiniest, little tasks and just focus on each one of those and literally act as if I was in slow motion.
So, I wrote in Seven Percent Slower that one of the ways I learned to actually do that was to exaggerate it in a huge way. To me, it felt like it was brushing my teeth in slow motion. I probably was, but it really helped because it was the opposite action. So, my amygdala is screaming, “Go fast, go fast, go fast.” And I’m like, “No, no, no, I’m going to go slower and slower and slower.” And it did change my state over time. And I was able to go out and start my drive and my exposure and panic all over again. But at least I was leaving the house at a level 5 instead of a level 8. But it did make it harder because when I slowed down, I would just feel all of the things. I just have to let them come and let them come. You know the deal, and your listeners, I’m sure, know the deal. So, it was tough, but it was also tremendously helpful to me. Slowing down was one of the biggest things that changed my situation, for sure.
Kimberley: Yeah. And the reason I think this is so important, this one thing and I love that you’re just looking at this one thing, is I think in that moment, for the listeners, we’re constantly talking about how to reduce mental compulsion. And I think the slowing down helps with that too, right? I think about there’s exposure, but there’s also the time before the exposure and after the exposure where you have to practice not doing the compulsion. And if you’re rushing, your brain’s rushing and everything. And so, I love that you’re even talking about before doing the exposure, you had to slow down.
Drew: Yeah. I mean really, before the exposure was exposure itself, there’s no doubt about that. And I had to come to the realization that like, well, the exposure right now isn’t the driving. The exposure is literally putting my shoes on right now while I panic, putting on my coat while I panic, brushing my teeth while I panic. And in Seven Percent Slower, I wrote about accidental emergency multitasking, which that’s the thing that I forgot. We were talking before we went in there. I forgot I wrote that. And I’m going through my editor’s notes, and I’m like, “I wrote that, how about that?” But that’s true because when you--
Kimberley: Good for me.
Drew: Yeah, right. Good for me. go through. So, I remember really thinking that, like when you’re in that crazy terrified state, I was trying to solve every problem at once. So, there was a lot of mental compulsion in there. I was trying to go through the drive in my head. I was trying to anticipate each turn. I was trying to beat back the panic before it even happened in my head. I was thinking about yesterday’s drive and how difficult that was. And slowing down, meaning it put things-- it made me focus on what was going on right now. So, it was also accidental or backdoor water down sort of ghetto mindfulness practice. I’ll take it though because it worked. It put me in the present moment and it took me out of emergency accidental multitasking mentally and physically.
Kimberley: I think it’s pure mindfulness, right?
Drew: Oh, it definitely was. And there was no-- I mean, I wrote about this in the book too. I’m not trying to read the whole book to you guys, but yes, it is part of it. There’s a whole chapter called Is This Mindfulness: Do I Need to Meditate to Slow Down. It’s literally one of the chapters. And well, it kind of is. If you start to learn to go slower, you will accidentally become more mindful without having to go through all the overwhelming things that sometimes people feel mindfulness is. “I have to become grateful and of the present moment, and I have to learn to appreciate the now.” No, you just have to slow down, and you’ll automatically mechanically become more mindful. The rest of the stuff is window dressing. It doesn’t matter. I wasn’t grateful for brushing my teeth at all, but I was mindful of it, and it got me out of those compulsions in that crazy, anticipatory anxiety cycle. Let me do the exposures more effectively.
Kimberley: Yeah. So, one of the things I love that you did-- and I actually did the homework. You’ll be so proud of me.
Drew: You did the homework. Did you use index cards?
Kimberley: Huh?
Drew: Did you actually use index cards, like I wrote about? I’m so old.
Kimberley: I did. Usually, when I read a book, I do not follow their instructions because I don’t like to follow instructions. It’s not my style.
Drew: I feel you.
Kimberley: My husband always cringes when I go to make an IKEA piece of furniture because I am bringing out those instructions.
Drew: It’s going to be an extra draw leftover. We just know it.
Kimberley: Oh, I could show you some photos. You would love, I tell you. But I did your homework. And this is what I thought was really interesting. So, I want to walk through. I’m going to try to be vulnerable here. I have noticed in the last week, since returning back from vacation, that my hyper-vigilance is going up a lot. I was noticing my anxiety wasn’t so high, but I was engaging in a hyper-vigilant behavior. I think mostly because I’m now thinking about COVID, how to protect my children, and all the things. When we were away, we were far, far away from anybody. We didn’t see anybody. So, I sat down, and I wrote the things that I do that I need to slow down at, right? And I’m just sharing it because I do the homework. I’m so proud of myself.
Drew: I’m proud of you too.
Kimberley: So number one is in the morning, I wake up and I sit up and I just go. I don’t ease into the day. And then you talk in the book about how speed is like an escape response, right? You don’t want to be in your discomfort. So, I thought that was interesting. These are ways that I’ve caught myself, right? So I jumped out fast. Like how can I not feel my discomfort about the day? Another one is I rushed during emails. And the big one, which I’m not happy about, is I multitask. Now I want to get your opinion on this as my dear friend, excuse me. Most people are probably multitasking, but why would multitasking be bad for anxiety?
Drew: Okay. So, I will preface this by saying, I used to think that my ability-- and I will multitask like a mofo. I’m good at it. I know that cognitive scientists will tell me that I’m not because there’s no such thing. We’re literally tearing down our cognitive models and building new ones every time we switch from test to test. I understand all of that. But I will tell you that I’m good at it anyway. I’m going to stick with my guns, right?
So, I wore it like a badge of honor. And when I have to, I can still do it. However, it absolutely fueled my anxiety state. There’s no doubt about that because there’s a sense of urgency that comes with multitasking. There really is. You are not present in anything when you’re trying to do everything. So, that really in the end is that. And multitasking is not just physical. It’s also mental. So, I’m answering an email while I’m thinking about the next email. I see your face. You know what I’m talking about. You’ve been there, right? You were probably there today.
Kimberley: Like I said to you, I’m so grateful that you wrote this because it’s so important. It’s so important for the quality of our life. Last week I was exhausted at the end of the week and it’s because I was rushing. I just know that’s why. That’s why I’m such a huge fan of what you’re writing.
Drew: As I was writing, things came out because I’ll be honest with you, when I thought of this as my own little mental device many, many years ago, I didn’t flesh it out. I just did it. You know how it goes. I didn’t invent a thing. But as I was writing about it, I had to think. And this speed to me looks like both an escape-- it’s both a fear response, sort of involuntary, and a safety behavior at the same time, like it keeps us from feeling the feels, right? So, yes.
And I think the other thing that multitasking does is it makes us sort of-- we can put our attention to the places that we want it to be at because they’re the easier things, even practically, like, I don’t really want to answer this email because this is a hard email. So, I’ll skip that one, mark it unread, and then go back to this one and I’ll just keep marking that. You know what I mean? So, it keeps--
Kimberley: You just described my whole week last week.
Drew: I hear you. The day I got to inbox 0, which was years ago – by the way, I’m not there anymore. Not even close – I was on top of the world. I was convinced like I’m now qualified to basically run the UN if I need to, because I’m at inbox 0. But I’m very guilty of that stuff where I was for a long time. I still fall into the habit. There’s no doubt about that. But yes, when I find my-- sometimes I do it intentionally because I need to, and there’s a time and a place for it. But when I find that I’m feeling extra stress, because one thing that I noticed about this book is that it doesn’t just apply to anxiety and anxiety disorders, but it applies to stress management in general, because I still use seven percent slower, I just didn’t remember that I was. And when I find that I’m feeling the effects of the stress, much of which I create myself by taking on so much, slowing down and stopping the multitasking, like close all the apps, run one app at a time, do one thing at a time, it really brings that down. It doesn’t solve all my problems, but it keeps me from being overwhelmed by the physical responses that come with stress. Why am I holding my breath? Why does my neck hurt? Well, I know why. Because I’m stressed, and I got to back off. It helps. It really does help to slow down.
Kimberley: It does. The final one that I listed, and I really want you to talk more on, is just a general sense of worrying, right? I mean, I think you can actually give me your opinion on this, but sometimes we do have to solve problems, right? We have to make decisions. This was a big one for us last week, is deciding whether we wanted to put our kids back in school or homeschool them, back and forth. Sometimes you do have to make those decisions, but there is a degree of just general worrying that happens. And then you can start to worry on speed at the highest speed ever. So, did you have to apply this to the speed in which you worried or try to solve problems? You’re talking about physically slowing down, but did you also apply it to mentally slowing down, or they go hand in hand?
Drew: That’s a really good question actually. And if I think about it, the way it worked for me personally, my personal experience with this particular method or whatever you want to call it, is that it was first the physical slowing down. But then I discovered that that started to spill over. So, when I was physically going slower and being more mindful and deliberate in my behavior, it became a little easier for me to recognize that I am literally thinking about 17 problems at one time right now. I can’t solve them all at one time. Some of them I can’t solve at all.
Kimberley: We could probably resolve or solve them already.
Drew: Exactly. And it really helped me clarify that habit that I have. I’m just going to think, think, think, think, think. I’m thinking all the time. I think anyway, but I was thinking very maladaptively in those days in a big way. I was a prisoner to my thoughts and the thinking process. And it really helped me break that cycle. It’s always important to me to say, slowing down and going 7% slower is not a cure for all of this or anything like that. It’s not magic. It was just one part of the puzzle. It turned out to be a big part of the puzzle for me because it unlocked a lot of things, but yeah, it did slow down my mental behavior too, my ruminating, my worry, my thinking.
Kimberley: Right. Yeah. I keep saying, I’m such a fan of these. And I think for me, I mean, you guys know I’m very well recovered, right? I’m mostly very healthy, mentally healthy. You might question me now that I’ve totally got that upside down. But I consider myself to be pretty level. What was interesting for me is, that for me is usually the first sign that you’re starting to go into relapse, right? When you start to speed up. So, that’s why I thought last week, I was like, the gods have all the stars aligned because I’ve come out of this very beautiful, long vacation where I’m managing my stress and everything. And the first thing my brain did when it got home was speed up. And if I hadn’t caught it being hypervigilant, I think I would have gotten snowballed, right? And I think it’s a great way, a tool to keep an eye out for your relapse as well.
Drew: Yeah. I mean, actually, these are hard things to catch, don’t get me wrong, because so much of it is automatic or it’s a little bit beyond. The initial speeding up is beyond our control. My assertion in the book is initially, you will probably automatically speed up, but you can catch that and then change it. It takes work. And I really talked about like-- in fact, today’s Instagram post is all about that really. Not that anybody has seen it because it’s a podcast for the future, but it was about that. Like, “Hey, look at these. Here’s 10 signs.” I did a 10 things posts. Now I’m disgusted with myself now that I think about it, but I have a list with 10 things like here is-- I think there’s actually 11, to be honest with you. But here’s a thing, if you find yourself doing this, if you’re stumbling over your words, if you’re shaking, if you’re dropping things, when you’re walking, if your stride length has shortened, because that’s what I would do. I have reasonably long legs, but I’d be taking these little tiny penguin steps because I was rushing like crazy, like running. So, there’s a bunch of practical things that you can really look at. This is what my rushing habit looks like. So I can be aware of those things and catch them and then start to slow down.
Kimberley: Right. And that was what you said in the book. Write them down, identify the behaviors in which you’re doing, which I thought was brilliant.
Drew: Thank you.
Kimberley: Yeah. Okay. I wanted to touch on, because I loved how you really talked about that, the side effect of slowing down is that you have to feel uncomfortable. Bummer, you totally ruined it.
Drew: I did. What a buzzkill.
Kimberley: We’re going so good.
Drew: Yeah. It’s true. I think that was one of the chapters. I specifically wrote an entire chapter about why you probably don’t want to slow down, right?
Kimberley: Exactly.
Drew: One of the reasons is that we view rushing around as some sort of badge of honor and achievement. If you run around like a speed demon, it must mean that you’re busy and achieving things, which is not true. But also, if you slow down, you feel all the feels, and we hate that. And I’ll use the word “we.” Humans are not really-- we’re designed to be creatures of comfort. We don’t want to feel crappy stuff. But you know that. I’m not telling anybody anything they already know. If they’re listening to Your Anxiety Toolkit, you already know this, but you have to move through the crappy stuff to get past the crappy stuff. And slowing down is a good way to allow yourself to do that.
Kimberley: Yeah, I agree.
Drew: Yeah. Accidental happy side effect.
Kimberley: I love that you brought this up. So, let’s go through like, okay, slowing down. You can even maybe share your own experience. Slowing down, for me, I think it’s not that I have to feel physically uncomfortable as much as I have to have a lot of uncertainty, right? I have to be uncertain, which is typically, at the end of the day, still just sensation and experience. For you in that, when you were practicing this during your exposures, what did you have to feel when you slowed down?
Drew: So for me, when I would slow down, I would feel the physical sensations of panic. The one sensation that never leaves me – it’s the memory of a sensation. It’s not that I feel it. I rarely feel it anymore – was the feeling of my heart thudding in my back. You feel like all my chest was pounding, but it would feel like it was beating so heavily when I was in a panic that I could feel it almost beating along my spine. It was a really uncomfortable sensation. And traditionally, when I would feel that, I would do everything I could to try to not feel that – wiggle around, change position, lay down, stand up – try anything that I could to not feel that.
One of the key things-- and I felt all the physical sensations, but that one sticks in my memory was when I started to slow down, I had no choice but to let my heart pound lead against my spine, and it was so uncomfortable. And I remember really just having to reason with myself as best I could like, “Just get through it for another 10 seconds. Just give it another 10 seconds. Just give it another 30 seconds.” And then it was just, “Just give it another minute.” And then it was like, “Oh, this isn’t so bad.” So, it was a gradual habituation to that where I stopped being afraid of it. And slowing down meant I had to feel that. There was no more shield against feeling it.
If I’m going to stand in the bathroom and slowly brush my teeth, I’m going to feel that. But I also heard the thoughts very loudly when I slowed down. And the thoughts would be panic-type thoughts, like, oh my God, what if it’s not anxiety this time? What if I’m having a heart attack? What if this is a stroke? It does happen to people. Even though I’m only 30 years old or whatever it was at the time, this can happen. What if, what if, what if? Those thoughts were already loud. And when I slowed down, I essentially turned down all the other sounds. So those thoughts were really, really, really loud. And I would literally have to practice. It forced me to practice like that could be, but it’s not likely. I would have to say that all the time. “That could be, but it’s not likely. It could be, but it’s not likely.” Yeah. And it just forced me to practice. So, I would feel the physical sensations and hear my thoughts so much louder. Hated it.
Kimberley: Right. Yeah. I’m so glad that you mentioned that. I mean, I can only imagine too. When we have those symptoms that aren’t textbook, like you feel your heart in your back, it’s hard to just let that be there, right? You and I have joked a lot, the old Instagram posts about like, these are the 12 ways to feel a panic attack. But when you don’t have something on that list and when you have something additional, that’s scary, right? “Oh, crap. I’ve got six things that aren’t even on that list. What does that mean?”
Drew: Here’s an interesting thing that you just made me think of now. The other thing that slowing down accomplished, and this was a happy accident also, is I like to look at it as imagine anxiety as a room. So, when your lizard brain, when your amygdala is in charge, it fills the entire room, so prefrontal cortex stuff has no room. It’s pressed against the walls. It’s being pushed out the door. There’s no reasoning at all.
When I slowed down, I actually made a little bit of room for prefrontal cortex to chime in. Winston and Seif, they will talk about wise mind in their writing. Wise mind had a chance to chime in where I was able to say, “Okay, Drew, yes, this isn’t on the list of the usual stuff, but you have felt things like this 10,000 times. And all indicators are: you’re healthy as a horse, you’re in great shape. It’s okay.” And it allowed me to tolerate that uncertainty a lot more because I was able to reason a little bit more. I was unable to talk myself off the ledge, but I was able to insert just enough reasoning because it gave me a little bit of room to work in. That helped also. I was able to actually do that, whereas before I was just frantic. That was like, “You’re okay. You’re okay. It’s okay. It’s nothing, it’s nothing.” But your amygdala doesn’t care. It doesn’t believe you. But in that case, I was able to actually say, “Okay, hang on. I felt this zillion times before. This is likely nothing. Okay, I can go with that. I’m going to roll the dice on that. I’m good with it.”
Kimberley: Right. You can see the trends that have been playing instead of thinking like it’s the first time it’s ever happened, even though it’s happened a million times.
Drew: Yeah. So, practicing slowing down gave me a little bit of space for that stuff to get a little foothold, a little handhold, and then it grew.
Kimberley: Yeah. So it’s interesting because I’ll share with you, a big part of my recovery has been considered what I have been calling a walking meditation. So, I did a lot of meditation training in the latter stage of my recovery. And I don’t love to sit and meditate because it’s uncomfortable, right? But what I love to do is this end practice of walking meditation. And so, I’ve often called friends and said to them, this is an accountability call. I have to do a walking meditation all day. And then when you’re writing this, I’m like, “That’s what I was doing. I was slowing down.” And I’ve been just calling it something different. So, I thought that that was really fascinating because in the Zen practice, you do a lot of walking meditation, right? Being aware slowly as you engage in the day.
Drew: Which is something that I think a lot of people have a hard time putting their brain around. In the beginning, I think it’s hard to do that – being mindful in motion. So, to me, meditation, I always say mindfulness to me is like meditation in motion. I don’t know if that makes any sense, but that’s--
Kimberley: It is what it is.
Drew: Okay. So, that’s the way I’ve always thought of it for myself. Well, firstly, I learned to meditate and then I put it in motion so that I can be meditative even in a meeting or on a phone call or driving my car. That’s possible, but that’s the thing you have to learn. But that’s part of slowing down also. When you do your walking meditation, you’re intentionally slowing down.
Kimberley: Yeah. I would even invite the listeners to think about when are you the most calm or coping the best is when you’re actually slowed down. For me, it’s when I’m with a client. When I’m with a client, I can’t multitask. I am so with them, and it’s their pace, which is not my pace. I can’t speak at a rapid, two times speed formula in session. And that’s where I feel the most connected. And that’s where I feel just wonderful. And there it is right there. It’s forcing me to slow down. So, I think it’s helpful also to look at where are you actually being slipped, where are you forced to slow down, and how are you coping in those situations.
Drew: Yeah. When you have no choice, you can actually try and remember, well, what does it look like for you? It’d be like, what does it look like when I’m in session? I just have to do that. When you’re not sure, well, let me just go to what that feeling is. And those things to me also-- the last chapter of the book is called Beyond Seven Percent Slower because to me, that skill that I developed accidentally years ago serves me well now.
So, one of the things in business that I get told all the time and people always say, the building could be on fire, and you’re just-- I mean, I was a dude that couldn’t leave his bathroom. I was so panicked and so agoraphobic, and they’re like, “No problem. You do this, you get a bucket, we’ll put it out. Everything’s going to be cool.” That’s the slowing down. And when you learn to do that, and you cultivate that skill, not only can it help you in your recovery journey, but it stays with you for a long time and it brings out the superpowers.
We sometimes think that rushing and multitasking is the superpower – not really. Slowing down and letting each of your individual strengths and skills shine through because they can because you’ve given them space, that’s where your real superpowers come out. That’s probably where you are the most effective as a clinician is when you slow down and you’re in that session.
Kimberley: Or as a parent or as a wife or as a human, everything, right?
Drew: Yeah. So, not to get all preachy about it, but I think it goes well beyond just the anxiety and stress thing. It’s a good life skill in general.
Kimberley: 100%. Okay. I have one more question.
Drew: Sure.
Kimberley: I’ve purposely not tried to go down the tips and tools because I just want people to actually buy the book and just go through it, like I did writing it down and really addressing it. But you talk about one thing that I wanted to talk about, which is the 92-second timer.
Drew: Okay. I have to search through my Ulysses app, where did I write about 90 seconds.
Kimberley: See, we just did this today. Let me tell you what I found was so helpful, is you said you set a reminder every 90 seconds to slow down.
Drew: Yes.
Kimberley: So, tell me, how important is that? Does it have to be 90 seconds? Was that a big piece of you retraining your brain? What did that look like?
Drew: Again, that was my own-- yeah, that’s right. I did do that, and I did write about it. So, I know we talked about it a little bit. That’s fine. What I did was, I had an original iPhone, like OG iPhone, and I had this stupid timer. And I had this timer in there for 90 seconds. I use 90 seconds. I don’t care what you use. I don’t think the number is magical in any way. But when I was getting into that panic state and when I started doing my morning routine to prepare to do my driving exposures, I would just set the timer and it would repeat every 90 seconds. And that silly little timer would bring me back to slow down, slow down, slow down. It was just a cue. That’s all. It was a silly little mental thing.
Do I think it’s critical for people? Some people might not need it. But if you do need it, I don’t see that there’s any crime in using it. And you could do it every 30 seconds, 60 seconds, every two minutes. It doesn’t matter. It was nothing more than an auditory cue to remind me to slow down, slow down, slow down, slow down.
Kimberley: The reason I bring it up is that has been crucial for me in all of my recovery, no matter what it is, is reminders. I think that it’s easy to go on into autopilot. And I love that you mentioned that because I am a sticky note fan. I talk about it in my book. I love reminders. That’s a crucial part of my existence. So, I just love that you brought that up because I think that we always have sticky notes like don’t forget to get eggs and you’ve got to make a phone call. And this is the opposite of that, which is like, “Slowing down, hun. Bring it down a notch.”
Drew: Kind of, because our reminders are usually to remind us to do things faster, now, don’t forget them, get them done. Whereas--
Kimberley: Urgent, urgent.
Drew: Yes, urgent, urgent. One of the funny things about this, the thing was, I don’t have my phone with me here, but the sound was that stupid submarine alarm, like errr, errr, errr, which you would think I would have made a silly little, I don’t know, like chimey, gentle thing. But I intentionally did the errr, errr because it was jarring. I needed it to jar me. And so, yeah, it was weird.
I did not have to use the 90-second timer for months and months on end. It was in the beginning. It became very helpful to me. And then I spread the timer out to two minutes and then five minutes, and then we just didn’t have to use the timer anymore. So, it was adaptive. I don’t want anybody to think like I live my life based on this silly timer going off all the time. That’s not the way it works.
Kimberley: And I get that. I think that that’s the cool piece here to the story you’re sharing. And I would make this a big piece of what I want everyone to take away, which is, like anything, this sucks to start. It sounds like for you and it has been for me, although, like I’m saying, I’m owning up to falling off the wagon here a little, which I’m fine with. It can be a 90-second timer to start. But then that’s where that muscle gets strong. It sounds like that for you, it’s pretty strong now.
Drew: Oh, it’s really strong. It’s automatic now. Yeah. It’s almost automatic, but again, that’s a lot of practice and repetition and really taking this to heart. It’s not an overnight thing. And I still make mistakes. I just catch them faster now. Now, there’s zillion things to do to get ready to launch this book. Yesterday, I fell absolutely into the trap. Totally did. Around three o’clock yesterday, I felt terrible. I was just agitated and all the stress stuff and anxiety stuff was like, oh, wait a minute here. So, I can see at least that that’s the benefit of it. It’s taught me to see what I’m doing and then correct it when I need to.
Kimberley: Yeah. And it’s great to have that. You’re modeling that beautifully, right? That it’s not going to always be the hardest thing. It’s like something that you can learn to strengthen, which I really appreciate. Okay, tell us about where we can get this amazing book.
Drew: Well, I think I made it pretty easy being a techie guy that I am. You could just go to sevenpercentslower.com, which you can either spell it seven or use the number 7, sevenpercentslower.com. We’ll get you right to the page on my website that tells you about the book, which should come out plus or minus September 15th. So, I don’t know when this podcast is going to air, but it’s either out or not. If it’s not, just get on my mailing list and I’ll tell you when it is out. And yeah, that’s how you got it. It’s nice, friendly, short. You read it pretty quickly, I’m sure. It’s not a giant 400-page monster like The Anxious Truth. It’s friendly, easy, I like to think funny, easy to remember.
Kimberley: It’s so great. I’m actually so in love since the summer. I read all these amazing, just like short, really goes straight to the point. I cannot stand books that tell you something they could have told you in 100 pages. So I love that. I think it was exactly what I needed to hear. So I’m so grateful.
Drew: Oh, I’m glad that you find it helpful, and thank you so much for giving me this little spotlight to talk about it and appreciate you.
Kimberley: Of course. I probably a hundred episodes got on and went on a big lecture about how everyone has to slow down. And this is perfect timing. I think we all need it right now.
Drew: Very good. Well, go get it. Sevenpercentslower.com. Hope it’s helpful for everybody.
Kimberley: Thank you, Drew.
Drew: Thanks, Kim. Anytime.
https://www.amazon.com/dp/B09G227B1Z/ref=sr_1_9?dchild=1&keywords=coping+skills+for+anxiety&qid=1631488551&s=digital-text&sr=1-9
In this week’s podcast, we talk with Allyson Ford about her journey with OCD and an Eating Disorder. Allyson shares how her journey with OCD began when she watched ERP SCHOOL, our online course for people with OCD. Allyson quickly realized that she had not only been working through an Eating Disorder but had also struggled with OCD. Allyson Ford shares these 3 main points on OCD Recovery:
- In recovery, don’t wait for the fear to be gone. You must take the action while scared/anxious for real growth to happen. It will feel counterintuitive but that doesn’t mean you are doing it wrong. ERP is terrifying and it’s worth it in the end. It’s so empowering to realize you can have anxiety and do the things you love anyways. Because it is so scary, you need a therapist that you can really trust- who is both skilled in ERP and compassionate/warm.
- Shame and myths about OCD keep us suffering for much longer than we need to. Two major turning points for me were learning about what real OCD is- I quickly identified signs and symptoms within myself since 8 years old. The next game-changer was finding a community of other therapists who live with OCD. I felt so embarrassed to be a therapist struggling with these issues- I felt broken and ashamed. It made work really anxiety-provoking. I attended Pure O Chrissie’s Gamechangers retreat and that changed everything for me. I suddenly felt empowered and hopeful; this propelled my ERP treatment forward.
- Learning and applying skills for intrusive thoughts was also a game-changer. Learning that everyone gets intrusive thoughts and that they don’t mean anything, learning mindfulness skills (bookshelf metaphor) for rumination and one-upping my thoughts/power stance were the most helpful. Knowing that the theme of my thoughts only points to what I value most was also helpful- it always boils back down to my work. I care so deeply about making a meaningful impact on my clients, and that seems to be what my OCD attacks the most!
Allyson Ford, MA, LPCC is an Eating Disorder, OCD, and anxiety therapist with lived experience. Allyson graduated with her Master’s degree from New Mexico State University and has since worked in a variety of settings including hospitals, schools, residential programs, and now private practice. Allyson provides virtual services throughout California and also does part-time work at The Eating Disorder Center with Jennifer Rollin.
Allyson has a passion for integrating social justice throughout her practice and has a podcast available on Apple and Spotify called Body Justice. Allyson utilizes ERP, DBT, CBT, ACT, and IFS in her practice. You can find her on Instagram at @bodyjustice.therapist and her website: www.allysonfordcounselingservices.com
This is Your Anxiety Toolkit - Episode 201.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Welcome back, friends. I am so happy to have this special time with you. Thank you so much for giving me your very valuable time. How are you all doing? Just checking in. I know it’s been a really hard year. I know we talked a lot last week about suffering and how to manage that. If you didn’t hear that episode and you’re struggling, please go back and listen. Hopefully, it will connect with you and land up with you in a way that is validating and kind and builds some space for you and some safety for you.
This is going to be a wonderful episode. It’s actually an interview I have done with somebody who I met through ERP School, interestingly enough. I am so honored to have this week Allyson Ford. Now Allyson is an LPCC. She is an eating disorder specialist and OCD specialist and anxiety specialist. She has lived experience, which she shared, in those areas, and she shares her experience of finding out that she has OCD, talking about her eating disorder recovery. And the cool thing is, like I said, she will reflect a lot on how ERP School, one of our online courses that teaches you how to practice ERP all on your own and learn about ERP – she shares how that was a big game-changer for her. So I’m so excited to share with you this amazing interview.
We talk a lot about the overlap between eating disorders and OCD. Even if you don’t have one or both of the disorders, I encourage you to listen because I think that there is some amazing story and I think it’s really cool to see stories of clinicians who have actually walked the walk. They don’t just talk the talk. So I’m so, so excited to share that interview with you.
Before we do that, let’s go ahead and do the review of the week, this week’s review. If you want to ever leave a review for your anxiety, you can. I would love to see it. We feature one review a week. This one is from StrongMom and she said:
“A big virtual hug. I don’t know how I found this podcast, but I’m so glad I did. Kimberley’s compassionate and honest conversations about anxiety and OCD provide tools and strategies for facing fears, anxiety, and BFRBs. Her friendly, nonjudgmental tone about the challenges are so helpful to me.”
Thank you so much, StrongMom. I love hearing that the podcast is helpful.
Before we get over to the main part of the show, we’d like to do the “I did the hard thing” segment. This is actually from someone you guys have had on the show before. This is from Alegra and she says this:
“I let go of someone who I really cared about because it was the best thing for me, even though it deeply hurt.”
I think that that is such an important “I did a hard thing” because sometimes we talk about it as just doing exposures, right? Facing our fear. But sometimes the hard thing is letting go of something. Sometimes the hard thing is setting a boundary with somebody. Sometimes the hard thing is listening to our own needs and following through with our needs. So I loved this submission for “I did a hard thing.”
Okay. That being said, thank you to you all for being here again. I am so grateful. I know I say it and I want to keep saying it. Thank you. Thank you for spending your time with me. I’ll head over to the show.
-----
Kimberley: Welcome, everybody. I am so excited for this episode. We have with us Allyson Ford. Thank you for being here.
Allyson: Of course. I’m so excited.
Kimberley: Yeah. Okay. So, let’s tell this story, and this is where I get so geeked out, is when I hear of people who’ve taken ERP School or taken one of my courses, and they’ll either post it on social media or something to say, “Oh, this was really helpful.” And then literally my life is like done. I feel so good. I’m so happy. And that’s how I met you, Allyson. So, I’m so grateful to have you here. Would you tell us a little bit about you and anything you want to share about your own recovery? I’ll ask questions as we go.
Allyson: Yes, absolutely. So, my name is Allyson. Like Kimberley said, I am a licensed therapist in California. I work primarily with eating disorders and anxiety, and I have my own recovery journey with an eating disorder. I just recovered from anorexia years ago, and it wasn’t until this year that I realized I also have OCD. For anyone that’s listening, it’s common to have both symptoms, symptoms of both. They really overlap. And so, I see it a lot in the clients I work with, and that’s what prompted me to take ERP School. I was looking for resources to become more trained to work with clients with OCD. And then through taking the course, I was like, “Oh my gosh, I have a lot of this.” And then I sought out an ERP therapist to work on things that were coming up for me, and it’s been really rewarding. And so, now I really enjoy working with OCD as well.
Kimberley: Wow. I have such big goosebumps on that. That’s so fascinating to me that you would be doing continuing education units for yourself and helping your patients, and then realizing you had symptoms yourself. When you took the course or when you considered this learning, what did you think OCD is compared to now what you know about OCD?
Allyson: Yeah. That’s a great question. Because I went to graduate school, I knew that OCD was obsessions and compulsions, and I knew that the compulsions had to take up a certain amount of time of your day. But what was unclear is, what is an obsession and what is a compulsion? So, I still had this stereotypical image of OCD being like hand washing and checking the stove. And yes, those can be symptoms, right? But I was thinking about this the other day and I wish they would change the name of OCD in the DSM. I wish it was like Intrusive Thought Disorder because obsession, to me, sounds like, you think of it as something you like. Like, “Oh, I’m obsessed with this.” We don’t think of it as something negative. Like, an intrusive thought is scary. It’s frightening. It’s so unsettling. I wish I would’ve known that it meant something totally different than just not just hand washing and cleaning.
Kimberley: Right. Exactly. Yeah. Like I said to you, that made my day to hear that because a big part of our mission is to help educate people who do think it’s like organizing your cupboards nicely and hand washing and lining things up evenly and so forth. So, was that a great realization for you? Or was that a sad realization for you to be like, “Oh, there’s more to it than this and maybe this includes me”?
Allyson: Oh my gosh, it was terrifying at first. Actually, when I was taking ERP School the first time, I was like, I knew this wise part of me was like, oh my gosh, yeah, these are some things you’re struggling with. But then there was a lot of not wanting to face that. So I think between the time I took ERP School till I actually got help was still like six months, and there was a lot of like reaching out to ERP therapists and then backing out. I was so scared because I knew through taking your course that I was going to have to face my fear.
When you go through one major mental health disorder in your life – going through anorexia, I was so terrified to go through something like that again. I’m so scared to have another label. Especially being a therapist, there’s like this extra stigma that we shouldn’t suffer. And so, that was a huge part of it. Just the stigma of having a mental health diagnosis again. But yeah, it was completely and totally scary.
Kimberley: Yeah. Isn’t that sad though? And I agree with you. I resonate so much with what you’re saying. Isn’t it sad that as therapists, we’re made to believe, or we take on the belief that we aren’t supposed to be human? For me, everyone on my account and my listeners know I had anorexia as well, but I did a tremendous degree of compulsive exercise, and it always felt OCD-like. As soon as I learned about OCD, I had a similar feeling of like, this is exactly what I used to do. I had a fear, and to remove this fear, I would do this one specific calculated move. And so, I get what you’re saying. You had already gone through treatment. Now that you know about ERP, did your treatment now look a little bit like ERP? Because for me, my anorexia treatment felt like ERP at the time.
Allyson: Yes. I would say it was a blend. It was a lot of facing the fears, reducing the compulsive behaviors, but then there was a huge relational component too. And that’s something I’ve been reflecting on with ERP, that sometimes I feel it’s missing in terms of ERP training. It’s like, we forget the fact that the relationship is the most important thing. Going through my own ERP, it being so terrifying, I needed to have a therapist that I really trusted that like, this is actually going to help me. So, yes, it was, I would say, a mixture of behavioral, but also just relational.
Kimberley: Yeah. So, true. So, if you’re comfortable sharing, would you share a little about the area of OCD that you have experienced?
Allyson: Yes. So, I’ve pretty much experienced all of them minus symmetry and contamination. But other than that, I’ve had pretty much all the themes. The ones that have been the stickiest in terms of the most impactful on my daily functioning have been real event OCD, which is – and you can correct me – but when something has actually happened and then you fear it like happening again, right?
Kimberley: Yup.
Allyson: That one was the one that actually propelled me to take ERP School. And then I’ve had harm obsessions, like fearing that I was going to hurt someone, fearing I would blurt something out really mean. That’s been a really big one for me. And then in the past, now that I know what OCD is, I can see that growing up I had fear or harm obsessions. Those were the main ones, but I’ve had all the intrusive thoughts.
Kimberley: Yeah. And that’s why I think it’s true. I agree with you, in terms of the word, obsession is very misunderstood. Isn’t it? It’s very much related to this unwanted experience. And I think that was a really different-- maybe you could share as well for a lot of people with eating disorders. Would you say that the eating disorder was an unwanted thought or a wanted thought?
Allyson: Yeah. So, that’s where it gets a little tricky. So, we talk a lot about egodystonic versus egosyntonic, and I would say in general, egodystonic is anything that you don’t like, right? You don’t want to be thinking that. With eating disorders, it’s tricky because you think you like it. But if you actually sit down and you ask the person, “Well, how is this impacting your daily life? Isn’t this behavior in line with your long-term values?” they will say no. I’ve never had someone say yes. Even though it feels like you like the thought or it feels congruent with who you are, it’s really not when you look at the long-term picture. I think that’s an important distinction to make.
Kimberley: Yeah. So important. And that’s why I love that you’re here because we don’t talk enough about eating disorders here on the show as much as I would like. I think that those little nuances are so important clinically to be able to understand. So, thank you for telling us. Okay, you took ERP School. What was your main takeaway? You obviously had the takeaway of like, “Oh, this could be a part of my symptomology,” but in terms of just what you’ve learned, what was the main takeaway for you?
Allyson: The biggest takeaway was that in order to get better, I had to face my fears. I had to take away the compulsions, which were mostly mental for me. And that was really hard to wrap my head around, like learning mindfulness skills to stop ruminating. I just thought everyone obsessively ruminated. So, I just didn’t know that that was a mental compulsion. So, identifying those and then retraining my brain. It was so hard. Like you said, I think in ERP School and in your podcast, you talk about how you might have to do it 500 times a day, like redirecting your attention back to the present – that was so true. It felt exhausting. So, those were my biggest takeaways – you need to face your fear and don’t expect this to be comfortable.
Kimberley: Yeah. I’m glad that’s what you took. I got goosebumps listening to that in terms of you talking about how exhausting it is. I’m curious for your experience, was the treatment of the OCD portion harder than the eating disorder? I mean, it doesn’t really matter, but I’m curious to know what that was like for you. It’s so exhausting, right? Facing your fear is so exhausting. So, did you feel that same level of exhaustion in your eating disorder treatment?
Allyson: Yeah, totally. I think it’s hard to compare the two and I’ve done a lot of reflecting on it. Let’s say, if I had to choose, do you want to go through the eating disorder again or the OCD, I think I would choose OCD only because it was so egodystonic feeling that I was really motivated to get better. The treatment took me a lot less time. Whereas with the anorexia, because our culture reinforces so many of the values of anorexia, you could say, it was really hard to change those behaviors because you’re fighting yourself and also everyone around you. Whereas with the OCD, it wasn’t that way. The culture wasn’t reaffirming the values of OCD.
Kimberley: Right. I agree.
Allyson: But I would say that facing the OCD fears, it felt scary. And I don’t know if it’s just because it was more recent. My anorexia recovery was like eight years ago, but it felt more intense. We were just ripping off the bandaid. Whereas with my eating disorder recovery, it was a lot more gradual. My therapist was like, “No, we’re going all in. I want to flood you with anxiety.” Oh, this was scary.
Kimberley: It really is. It really is. You know what, I’ll tell you an interesting story. A little bit off. But I was talking with a really, really somewhat high-profile influencer on social media the other day. I was actually asking a question about something specific. She had looked at my account and she’d said, “I find it interesting--” we were talking about microlearning, which is ultimately like teaching in very short, small 32-second blocks. She said, “I noticed that you talk a lot about disorders and you keep telling everybody how hard it is.” She said, “I find that a little depressing.” But that was just some feedback that I had said to her, my response was, “I’m in the trenches with people at the beginning. And if I don’t tell them, it’s going to be hard, they’re going to question themselves on why it’s so hard.” I thought that was such an interesting reflection of someone who’d be like, “Your account is depressing.” But I had only ever seen it through like, no, that’s validating. So, I 100% agree with what you’re saying.
Allyson: I find that very validating because yes, when I went through my own ERP, I already knew it was going to be hard from taking your course, from reading your content, right? But until you’re in that moment doing ERP, you don’t realize how hard it is. If I was going into it with the expectation that it was going to be easy and super cheery and helpful, I would have collapsed. The fact that I knew it was supposed to be hard I think definitely helped, and my therapist validated that too a lot. Yes, if it’s scary, if you’re flooded with anxiety, you’re doing it right. That was the biggest difference from anorexia recovery because an eating disorder recovery, I think we focus so much on coping skills for anxiety that we miss the point that we can teach clients just to tolerate the anxiety. You don’t have to do anything about it. That was a game-changer for me.
Kimberley: I agree. It takes all the wrestling out of the work, doesn’t it?
Allyson: Yeah.
Kimberley: Yeah. So, I just thought that was a really funny story because I’d never once considered myself to be having a depressive social media account, but I totally get that perspective for people. I think it’s because they’re not looking at it through the lens of, if you have to face your fear every day, you do need that reminder. And I really appreciate you mentioning that. Was there anything that surprised you during your original training in ERP? Was that shocking to you? Or did that actually be like, “Oh no, that sounds bright”?
Allyson: I think once I was taking the course, I realized, yes, this makes sense. It wasn’t necessarily shocking, but learning about the OCD subtypes, that was the most eye-opening to me of, “Oh, this is what real OCD is, not everything we’ve been conditioned to think it is.” So, that was I think a huge turning point. Then I could pinpoint like, “Okay, where am I struggling the most? How is this manifesting for me? What do I need to do about this?”
Kimberley: Right. Yes. Will you share with us some of your exposures and what that was like for you? Walk us through.
Allyson: Sure. Yeah. So, I think the funniest exposures in terms of listeners listening to this would be the blurting out ones. And I say fun in a sense that they sound funny, right? Because OCD does not make sense. It’s not logical. It attacks things that we know we care about, but OCD makes us question ourselves. So, when I had these fears that I was going to blurt out, people’s like-- let me backup.
Social justice is very important to me. And so, the fears of blurting out were fears that I was going to blurt out, people’s like marginalized identities. For anyone that doesn’t know, OCD attacks what you care about most. So, it felt so scary to me to have these thoughts of blurting out these obscenities to people. Some of the exposures that I would do, that my therapist had me do, was first like watching videos of people blurting out stuff. I had this fear that like, what if my brain just broke and I started blurting out stuff? So, she made me watch videos of people with brain damage and things like that. And then I wrote out a lot of scripts, writing out my feared outcome, listened to that 30 minutes a day over and over. And that was terrifying. And that I got from ERP School.
And then the other one, I think what helped the most was my therapist had me write out my feared outcome on sticky notes and put them all over my room. So, when I woke up in the morning, I was flooded with anxiety, just seeing all the intrusive thoughts all over my walls. If you would have walked into my room, not knowing I was in ERP and stuff, you would just think I was a total weirdo.
Kimberley: That’s commitment, right? You were so committed to your recovery. I’m so proud. That’s so cool.
Allyson: I just wanted to get it over with. They say this is going to work, so I’m going to trust these professionals. I know the science myself. I was just so motivated because living with OCD is harder than going through the treatment.
Kimberley: Yeah. So, I have a question, which I think is a question that my clients commonly ask, and you’ve gone through it, so I’d love to hear your thoughts. Often you are really into social justice. So I’m sure the idea of saying these words was horrible, right? It went so against your values. So, when you were doing the exposure, was it hard for you? Did that feel like you were going against your values to do the exposure? Or how did you manage that piece? Because I’ve had clients say or people from ERP School say like, “But I don’t like these words. I actually disagree with these words.” Maybe it might be a racist word or so forth, then that was really, really upsetting for them. And so, the idea of doing an exposure to something that they wholeheartedly do not value and in fact, they are disgusted by is really painful. So, how did you navigate that?
Allyson: Yes. Well, to answer your question, yes, that was very hard. And higher up in the exposure hierarchy, I actually had to write out the obscenities while I was talking to someone. So, I’d be like, let’s say, I’m talking to you right now, and then my exposure would be taken on a sticky note or on my phone, type out the word that my OCD is saying I should say. And it felt so opposite to my values. It felt so wrong on every single level. Even just remembering it, I’m going to get a sick feeling in my stomach. It does that disgust, that guilt, that anxiety. It’s so all-consuming. But I think I had to have blind faith and trust the process, as cliché as that sounds. Trust that this is supposed to habituate my brain and not I can tolerate it. So, yeah, it felt totally opposite. But then once it started getting better, meaning it started causing me less anxiety and less feelings of disgust, I started believing that like, “Oh, this is what I’m supposed to do.” And it was easier to keep going with it. But that first week was excruciating.
Kimberley: Yeah. I bet. I’m so grateful you did the work, but I’m sorry you had to go through that, right? It’s not easy. Yeah. And you’re right, and we share this all the time, is it does attack often the things you value. Moms have to do pedophilia exposures they are disgusted by, or the dad has to do harm. I’m not picking a gender for any reason, but just using those as examples of a dad who have to have harm exposures and have to expose himself to his own aggression. And these can be so painful. So, I love that you’re sharing-- particularly, I love that you’re sharing about the social justice piece because I’m seeing that a lot in my practice. Because of how aware we are now of making sure that we are politically correct, or even the Me Too movement, I think a lot of people are reporting anxiety about if they said something or if they touch somebody inappropriately. I think it’s becoming more and more prevalent.
Allyson: Absolutely. And that was something I really had to learn in therapy. There’s all these cognitive distortions with OCD and just like thinking errors, right? And one is that we are hyper responsible for everything we say and do, and that we have to say things perfectly, it’s very black and white. There’s no room for error. And that was a part where I had to accept that just like everyone, I’m imperfect. Sometimes I am going to have a thought that is not aligned with my values of social justice. But that doesn’t mean I’m bad. And it’s learning that that’s okay. I’m only human. It’s not my job to save the world.
Kimberley: Right. And that we can be imperfect, right?
Allyson: Right.
Kimberley: Yeah. I think that is so, so true. So, so beautiful. I’m so glad that you mentioned that. Okay. So, tell me a little bit about skills. Actually, I wouldn’t be totally happy as we go if you want to compare and contrast the skills you used in eating disorder treatment compared to OCD treatment, but what are some of the skills that you either learned through CBT School or ERP School and through your therapist? What were the skills that got you through the most?
Allyson: Yeah. So, I can tell you the top two that were the most impactful, because my compulsion is where mostly mental – learning not to ruminate and using mindfulness to do so, which you explained very well in ERP School. And so, basically, this is how I pictured in my head, is where let’s say, I’m talking to you and I’m starting to get intrusive thoughts that I’m going to blurt out something mean. I picture this little monster in my head, which is the OCD, and I just in my head and say, “Oh, okay, hi, you’re there.” Acknowledge it. But then come back to the present, like constantly refocusing my attention to the present. So, not trying to push it away, not trying to figure it out.
That was a huge game-changer for me because when you’re caught up in your thoughts trying to figure it out, then you’re totally removed from the present. I wouldn’t be able to focus on what you’re saying. But to learn like you can think four things at the same time. We do that all the time anyway. I could be thinking about my lunch right now and I’m still focused on you. So, learning that was huge. And I will say it wasn’t easy to learn though. In the beginning, I had to do it over and over. And then eventually, I feel like it’s like a muscle. Your brain gets more used to it. And now I can do it pretty easily. But it took me a while to get there.
And then the other one, it was one-upping my OCD, and you talk about that in ERP School. Also, I went to Chrissie Hodges’ Gamechangers event and Alegra Kastens was talking about one-upping and just giving examples of how she does it in her daily life. I started using that and just really standing up to my OCD.
So, for listeners, what that means is, let’s say I get an intrusive thought that I’m going to blurt out something really mean to Kimberley. What I would say to my OCD is, “You’re right. I am. I’m going to do it and it’s fine. I’m just going to do it. You’re right.” And just like, kind of what you would say to a bully, just rebel. And when you do it, standing in a really confident posture really helps me, just overpowering it. “You’re right. I’m going to blurt out today. I’m going to ruin my reputation. I’m going to go down in history as the worst person ever.” Just make it really dramatic.
Kimberley: Yeah. I love it. I do. I do. And I do agree with you on the posture piece, right? I think that power pose we take against OCD or fear can make OCD or the fear back down pretty quick. Not that it makes it go away, but it means you are in charge, not him.
Allyson: Exactly. Because OCD and anxiety and eating disorders make you feel really small and powerless. When we feel that way, our body reflects that. And then brain chemicals change that make us feel more like that. So when you change the bodily stance, yeah, it really does work.
Kimberley: So curious, did you have that fear about the podcast today?
Allyson: No, actually I didn’t. I mean, as we talk about it, the thoughts can come up, right? But I didn’t go into it that way, which is incredible.
Kimberley: Yeah. Would you agree that had you not gone through your own exposure and response prevention, this setting would be something that would be triggering or is it more just face to face with people in your daily lifestyle?
Allyson: It totally would have been triggering. Yeah. Because it’s any situation that’s a bit anxiety-provoking or that’s really important to me. So, this is very important to me, right? Or talking to people in my life that are super important. It would come up in those moments. Or with the pandemic, I hadn’t seen family for a long time. Then when I finally saw them, I was a little bit anxious and I had these thoughts towards them. So, it’s any situation where I feel anxious and sometimes OCD feels like it could be completely random.
Kimberley: Right. Oh, it’s so good. I like it. I just cannot tell you how rewarding it is just to hear you say. I just love when someone will say like, “Oh, I didn’t know I had OCD,” until they found ERP School or something or a podcast or something. So, I just love that information is getting out there. Before we finish up, is there anything that you really want the listeners to know? I know you’ve already outlined these main key points, but is there anything that maybe we’ve missed or you want to reinforce a message that’s really important for you that they would hear?
Allyson: Yeah, absolutely. I think just reflecting on the different journeys of anorexia recovery and OCD recovery, I will say that it is so important to learn that you can tolerate discomfort and anxiety because in anorexia recovery, there was so much focus on coping skills that I use so much distraction and reassurance and then all the compulsion to deal with recovery that I think if I had learned, that you can just tolerate anxiety, you can have a good day with anxiety, that would have prevented so much pain, mental pain. Because now when I get anxious, I’m like, “All right, I’m going to go to work just today, I guess,” or “All right, I’m going to do this anxious,” but it doesn’t automatically mean your day is going to be terrible. And that’s what OCD, anxiety, those disorders all try to make you feel that way. And it’s so empowering to know you can do this. Yeah. You can be an anxious mess and still have a great podcast.
Kimberley: 1000%. I love that message so much. I could just keep going. I’m actually really, so I’m going to, of course, give you a chance to share about where people can find you. But all I want to hear is I love hearing the contrast between the eating disorder and the OCD treatment. I think that that’s something we’re not talking about enough. We should propose a conference talk or something on that because I think it’s so important for people to understand those differences and why they’re so important and how ERP can actually work for eating disorders as well. So, so cool. Tell us where people can hear more from you. I know you have your own podcast. Tell us all the things.
Allyson: Yeah. So you can find me on my podcast. It’s just called Body Justice. It’s all about social justice, eating disorders, anxiety, all of that. And then on my Instagram @bodyjustice.therapist, and then my website, www.allysonfordcounselingservices.com. And on TikTok too, @bodyjusticetherapist. I’m getting into it.
Kimberley: I can’t get into TikTok, but I will watch and learn from you.
Allyson: It took me a while, but now I’m like, this is a bit easier than Instagram.
Kimberley: Oh, is it?
Allyson: Yeah.
Kimberley: Well, I really am so grateful for you. Number one, I’m so grateful that you’re out now as a clinician, training other people how to do this, which makes me so happy. We need more OCD therapists. So, that makes me so happy. But I’m also just grateful that you’re here to share this story. I think it’s so important that people hear your story and, yeah, I’m just so happy.
Allyson: Yes. I’m so grateful too, Kimberley. You’ve been huge in my journey to recovery from OCD. So, super grateful to talk to you today.
Kimberley: I’m so happy to hear that. We’ll be hearing more from you in the future. It sounds like you’ve got some amazing things to share. So, keep up the good work.
Allyson: Absolutely. Thank you.
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 200.
Oh my stars, you guys, Episode 200. So exciting.
Welcome back to Your Anxiety Toolkit. I am so thrilled to have you here for Episode 200. Oh my stars, you guys, this is a huge deal for me. In fact, let me set you up for today’s episode.
So, in Episode 100. We actually invited all the guests that we had previously had on the podcast and we had a celebration. If you want some fun, you should go over there and listen. It is such a wonderful episode.
I was thinking about what I wanted to do for Episode 200, and I’m not going to lie, nothing landed. Nothing. I just couldn’t bring myself to throw a huge party for it. And I think that’s what I wanted to talk with you guys about today in this episode, which is, who’s suffering? Who’s struggling? Who is having a hard time? Because I know I am, and I’m guessing you are in some way or another. I wanted to use this episode as just a time where we can talk about suffering and we can talk about what that looks like and what that means and what we can do when we’re struggling. And so, let’s talk about that today.

Before we do that, let’s first do two new segments. In fact, one is new and one is a return of an old segment we used to do. And the first one is where I would like to read you a review of the week for the podcast.
This week’s review is from Katie. Thank you so much for your review, and for all of you for writing a review. You guys do know that I’m giving away a pair of free Beats headphones once we hit a thousand reviews. We have a long way to go, but I am committed to getting there. And so, in the meantime, let’s celebrate each of you as we go.
Today’s review is from Katie and she wrote: “This podcast is a great resource that has helped me before I was brave enough to seek treatment. It’s nice to know that I am not alone. The tools and conversation are authentic, helpful, and hopeful. Grateful for Kimberley’s generosity in sharing.”
Thank you, Katie, for leaving a review, and thank you to all of you for leaving a review on the podcast. It helps me to get reach ultimately, and that helps me to help more people with this free resource.
Alright, so the second part of the podcast is a return to the “I did a hard thing” segment. Now, we have actually upgraded this segment. And what we’re going to do from now on is I have a form on my private practice website, where we launched the podcast. It’s called KimberleyQuinlan-lmft.com. If you go over there and you click on Podcast, right there is a way to submit your hard thing. And so, we used to do it on social media and we used to do it via email and it was very, very messy. And so now, you get to submit your “I did a hard thing.” We will take a look at them and we will do one per week. I am so excited.
I really believe that the “I did a hard thing” segment is literally the basis of this podcast. When people tell me or they DM me or they message me, or they tell me in person that they did a hard thing, they tell me as if this is a new concept to them that they’ve never, ever been encouraged to do. They tell me as if it’s life-changing. And that’s why I really feel like this is the core of this whole podcast, which is to come together as a group to do hard things. And maybe the hard thing isn’t something that’s hard for other people. That’s totally okay. That’s the whole point. If it’s hard for you, it’s hard for you. And I love celebrating that because sometimes, out in the world, we don’t have people to celebrate with. And I think that needs to be such a huge piece of the work that we do, and it is such a part of the work that we do here.
So, to get us started, I’m actually going to do the first one. Now, I want to encourage you to think of your hard thing as just something that’s hard for you. And then we can talk about here in a second what that may mean.
So, my hard thing for this episode is this, and I’m so excited to tell you this, is that Your Anxiety Toolkit Podcast hit 1 million listens. 1 million downloads, 1 million times people listen to this podcast and I could not be more excited. And this is why I think this is so important, is because as I went and I learned of this wonderful achievement, immediately, I heard a voice that says, “Yeah, but such and such got there in way quicker time,” or “Yeah, but I know that some people who have way more successful podcasts than you do, they’re going to look at that and they’re going to be like, ‘Oh wow, just a million?’” And immediately, that voice came in.
And so, what I want to encourage you to do is catch that voice when you recognize that you’ve done a hard thing. Because when you can catch the voice, you don’t have to then engage with the voice and go, “Yeah, you’re right. No point really celebrating that because other people got there easier and faster and better and all the things.”
So, here today, I am going to celebrate this milestone. Thank you so much for you guys for supporting me because I never would have gotten there without you. And I want to invite you to go over. I will put a link in the show notes below where you can submit your hard thing, and there will be no judgment here. If your hard thing is getting out of bed, that is a massive win. If your hard thing is going to therapy like Katie’s was, then that is amazing. If your hard thing is doing the 10 out of 10 exposure on your hierarchy list, then that is amazing. And I want to make sure every single week, we are celebrating one of you at least with your “I did a hard thing.”
Okay. So, those are the two segments we needed to get started on. Let’s talk about suffering.
So, here it is, you guys. I know you guys know a lot about my story and I was so lucky to have this beautiful summer where we got away, and I had so much time to heal and rest and be with my kids and it was magical. I’m not saying that to brag. I’m just sort of saying that if you have 10 minutes even to spend with yourself and rest, I cannot promote that enough. The resting is so important when it comes to our recovery.
And then when I returned back to LA, we had to come back and prepare for my children to return to school. The thing that really got to me is– let me just share with you really quickly about our vacation really quick – we decided to leave LA for the summer. We took seven weeks and we got in our SUV and our raft. We didn’t get in our raft. We towed our raft and we brought that around and we traveled eight states over seven weeks. We rafted 65 miles as a family. It was wonderful. We rested, we played, we sang a lot of annoying children’s songs. We listened to a lot of audiobooks, so that was wonderful.
But it was really interesting as we left Oregon down into California. The minute we crossed the border, all of a sudden, we were hit with smoke, and it was like driving into the apocalypse. Smoke was everywhere. We couldn’t see 100 feet in front of us. And the closer we got to LA, the more I noticed my anxiety rising and my sadness increasing and dread and all the feelings. And then I got back to LA and really wanted to spend some time readjusting with my family. But all I could think about was, wow, everybody is suffering so much – COVID numbers and the fires and earthquakes and political issues.
I wanted to really slow down for you guys enough to validate your distress to validate the suffering and struggles you have. Chances are, you’re dealing with all of that on top of some type of mental struggle or medical struggle. And so, I wanted to first just give you permission to take some time and validate that this is hard.
I find that when I speak about suffering with my patients and my clients, a lot of them often diminished their suffering by saying, “Yeah, but other people have it worse,” or “My thoughts are irrational, so I shouldn’t be this distressed,” or “I have a home,” or “Whatever it is, I shouldn’t be sad.”
But I want to remind you of this core important fact, which is, all forms of suffering are enough and are valid. Don’t get into the comparison trap of who’s suffering more and who deserves to suffer more and who deserves help and who doesn’t. You deserve help. This is a very difficult time and we must hold our suffering and our struggles in a warm, nurturing position.
You know, you guys, I always sort of make the joke of imagining you are holding a beautiful, yellow baby chicken and their little bones are like, oh my gosh, toothpicks, but not like toothpicks because they’re so frail. And if you were to hold them, you would be so gentle with the baby chicken. Your touch, your facial expression, your warmth in your voice would be so gentle. I want you to hold your struggles as silly as it seems like a baby chicken. Beautiful, tender, warm, kind, respectful tenderness. I really hope that you can do that.
The other thing I would encourage you to do – and I don’t know if this will help you, it was incredibly helpful for me over the last two years – is to continue to remind yourself that suffering is a part of being a human. Often I get caught – and this was a big lesson for me at the beginning of COVID, which was a part of me, and also when I got diagnosed with postural orthostatic tachycardia syndrome, I know a lot of you have struggled with this when you’ve been diagnosed with a mental disorder, whether that be OCD and eating disorder and anxiety disorder, a depressive mood disorder – is we want to sort of stomp our feet and say, “This shouldn’t have happened to me.” And by all means, please stomp your feet. Please have as much time to grieve that as you need. Again, there’s no reason for us to invalidate our own suffering, but for me, it was really important to remind myself that humans do suffer.
As COVID happened, I had to keep reminding myself, COVID, while it’s a huge issue and as harming so many people, is-- and I noticed I was like, “This shouldn’t be happening. This is wrong.” And I had to keep reminding myself, like, who says, it’s wrong? Who said it wasn’t supposed to happen? Who said that we were supposed to have a life that’s only easy? Who said that we weren’t supposed to struggle with mental illness? When it comes to mental illness, that’s what we would consider internalized ableism, which is, this idea that we should always be in tip-top shape. We should always be thin. We should always be smart. We should always be able. We should always be capable and handle things well. That’s just not human. It’s never been that way. it should never be expected to be this way. You’re allowed to suffer. You’re allowed to have troubles and struggles and pain, and you’re allowed to stumble as you try to navigate that.
And so, what I really want to remind you out when we talk about suffering is really taking away expectations that it was supposed to be easy and that it was supposed to be a free run. Now, I put in a caveat here, which is, you don’t deserve this either. You don’t deserve this suffering. It’s not a form of punishment. I know a lot of people come with that belief that they are being punished for something bad they’ve done. You didn’t do anything wrong. You didn’t ask for this. This is painful stuff. And I really hope that all the compassion practices that we’ve talked about here on this podcast have given you the tools you need to support yourself as we continue to suffer and struggle.
Now, there’s one last thing I want to mention, and that is hope and faith. I have had to wrap my head around these concepts during the last three years. How can I be hopeful when we have global warming or pandemics or hate against minorities? How can we be hopeful about this? This is where I’m going to encourage you to find hope in you, find hope in the community and the support around you. This community, if you haven’t got a supportive community, look and focus in on this community and the people who are doing the hard things and who are searching and struggling and working through what it’s like to have a mental illness. Bring your attention to those who’ve done what you are wishing you could do. There are so many advocates, you guys. I look to them every day. People who have lived experience, who have been through really difficult things and have come out on the other side – I look to them for hope and I use them as a little lighthouse for where I may need to go next. And I hope that I can be that for you.
But I really encourage you. As you’re navigating your suffering in this time, I really encourage you to look to the people who are doing things the way you wish you could and just use them as your shining light. You don’t need to do what they’re doing. You don’t even have to stop there but use them as a beacon of hope that together we can get there and that you will get there, and that together we can hold space for each other’s pain tenderly, compassionately, respectfully. That is my hope for today.
So, that being said, Happy 200th Episodes. I always end the episode by saying: It is a beautiful day to do the hard thing. And I know you’re all struggling. I’m struggling. I get teary just talking about this with you, but every day I say to myself, this is a beautiful day to do the hard thing. I’m just going to do one step at a time. I’m going to ask for help. I’m going to find my community. I’m going to celebrate my wins. if you can maybe put your attention there, I hope you can – maybe that will make the day a little lighter and the suffering a little less difficult to bear.
Have a wonderful day, you guys. I love you. I will see you for the next hundred episodes or more, the next million listens or more. I really am just honored to be on this journey with you.
Have a good day.
This is Your Anxiety Toolkit - Episode 199.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Welcome back, everybody. Oh my goodness, I am so excited about this episode and so deeply honored. So, for those of you who know me, you know how completely-- oh my gosh, I get so excited about meeting my mentors – people who have taught me so much as a clinician, who have taught me so much as a human being. Today’s one of those days, you guys, I am so excited and so grateful to be able to have, like I said to you, my biggest mentors on the podcast.
Today, we have on the podcast talking about shame, Dr. Christopher Germer. So, if you guys may remember, I did interview Kristin Neff before COVID about self-compassion, and Christopher Germer, who we have today, has co-founded the mindfulness self-compassion concepts and tools. They have workbooks, they have trainings, a website, and the work they’re doing is so important. I strongly encourage you to go over and check out the work that they’re doing, because it is life-changing.
But today, what I’m so excited about is sharing with you a conversation I had with Christopher Germer about shame, and he really breaks down all of the things we need to know about shame. We talk about some things that I myself have still got a lot to learn. Some of the things he said today – I had to do everything in my power, not to be like, wait, stop, I need to be able to think about that for a second. I need you to say that again, because he just drops so many truth bombs, and he is so amazing.
So, I’m going to stop going on about how excited I am because I have a total fangirl experience right now. I literally just got off the phone with Dr. Germer, and I’m going to share this with you. So, I hope you enjoy it.
If you are somebody who has struggled with shame, you are going to love this episode and take a lot away because it is such an important part of all of our recovery and all of our well-being. So, enjoy the episode, everybody, and I will see you all next week.

-----
Kimberley: Welcome. I am so honored, and I have such deep respect for today’s interview guest. We have today Dr. Christopher Germer. Thank you so much for being here.
Christopher: Thanks, Kimberley. Great to be here.
Kimberley: So, I’ve actually been dreaming of having you on for some time. I really wanted to hear your thoughts about shame. I was at a presentation or a training you did in December, right before COVID started, and I loved what you had to say. So, this is the topic of today. Can you share with us, just give us a brief description of what shame is?
Christopher: Well, shame is probably the most difficult human emotion. Shame is probably the most hidden human emotion, which is also why it’s so difficult, because if we can’t see it, we can’t work with it. But shame is primarily-- it has two main aspects. One is it’s a self-conscious emotion, which means we’re kind of seeing ourselves in the minds of others, and there’s also negative self-evaluation. So, what we’re seeing in the minds of others, it’s usually some scorn, something negative. So, those are the two main characteristics of shame.
Shame also has a kind of-- there’s kind of a global negative evaluation involved. In other words, we don’t just think a part of me is kind of needing to be tweaked a bit. It’s like, I am fundamentally bad or unworthy or incompetent or helpless. So, there’s a kind of a global evaluation. So, that’s shame.
But at the end of the day, what shame really is an attack on the sense of self. So, guilt is a criticism of one’s behavior. In other words, I did something wrong. Shame is “I am wrong.” So whenever there is a self-attack, there’s usually an element of shame involved.
Kimberley: Right. And I think that’s so interesting that you say, because it’s such a huge component of someone who’s struggling with a mental illness, or even just emotions, in general, is a lot of us when we’re having a hard time, we move immediately to like, “There’s something wrong with me.”
Christopher: Yeah. So, shame can either be the cause of different forms of mental distress or the consequence. So, when we think badly of ourselves because we’re struggling, say with an anxiety disorder or depression, then that’s an element of shame – thinking badly about ourselves, right? The self-attack. Or if we get negative messages from the culture, like if what we’re struggling with, it’s stigmatized or if it’s a burden on somebody in our lives and they start to criticize us for what we’re going through.
So, in that way, shame is a consequence of some internal distress, but it can also be a cause. If we are beating up on ourselves or something that happened to us in childhood, and inevitably, for example, if we suffer a lot of criticism or neglect or abuse in childhood, we basically blame it on ourselves and we carry shame through our lives.
Shame takes the form of self-criticism. It takes the form of self-isolation. It takes the form of self-absorption. Any of those ways of being have a serious effect on our mental health. If we isolate ourselves, then we get lonely. If we criticize ourselves, we can get anxious or depressed or anything. So, shame can be a cause or a consequence of mental illness, mental distress, and certainly anxiety.
Kimberley: Right. I love that you identify that. So, I think a lot of us understand that you would experience shame and have some self-criticism in relation to that. Can you share a little bit about why you think we would alternatively isolate?
Christopher: Well, it just goes along with the shame.
Kimberley: It just happens.
Christopher: Isolation is a hallmark of shame, but maybe one way of looking at it is evolutionarily. In other words, we have shame because in human evolution, it served the function, and the function it served was it kept the tribe together, and tribes that stayed together survived. So, when somebody sort of broke the rules, it jeopardized the tribe, it jeopardized the individual, and that wasn’t good.
So, what shame is, is a really intense emotion that we feel when we break the rules, and then the tribe excludes us. And that became hardwired in us through evolution because those people who basically felt shame stayed in the tribe and survived. So, therefore we have shame.
The problem nowadays is that we could feel shame for just about anything that has nothing to do with survival. We can feel shame because my body type or my sexual orientation or gender identity, anything we could feel.
The interesting thing, Kimberley, is that actually, we are more likely to feel shame when we are being devalued in a social context than when we do something wrong. It’s quite possible we do something wrong, even something that violates our own standards. And we just feel just a little bit of shame. But when people treat us in a devaluing way, then we have a lot of shame.
So, the question was isolation. Shame has always been associated with isolation. But what’s really interesting is that in the tribe and among our ancestors, the way they got us back into the tribe, fortunately, was by making us feel bad, not by beating us up. If they had to beat us up to get into the tribe, that would be not good for the survival of the tribe. So, we learned the fine art of shame, and it feels like we’re getting beat up and we just want to get back. We want to get back into the good graces of our friends and so forth.
So, bottom line is that it’s just the central part of shame to feel extra – kicked out of the tribe alone, desperately alone.
Kimberley: See, that’s so fascinating that you said. I’m going to have to relisten to this, this term around like, it’s true. We could be physically hurt, but there’s that emotional when someone says something about us and they attack us emotionally. That can be the most painful, heavy load. That can create a cycle of shame and all of those and isolation and criticism. That’s so interesting. I’ve not heard it being explained that way. Can you tell me about self-absorption, though?
Christopher: So, in a moment of shame, two things happen. One is we are stopped dead in our tracks. There’s like a startle. There is a fear response. Sometimes there’s like a moment of panic. So, that goes with shame. And then there’s instinctive turning inward. This also makes good evolutionary sense because then the idea is you would turn inward, and then you would take inventory of what you did wrong and then fix it.
So, that turning inward is a part of shame, but it’s only helpful, Kimberley, when it’s mild shame. In other words, if you, I don’t know, mistreat somebody, and then you stop, you turn inward, you realize what you did wrong. And then you basically stop feeling ashamed, and a little bit, you start moving a little more into guilt, and then you apologize, right? People in the midst of shame, they can’t apologize. They’re too self-absorbed. But when it turns to guilt, then you can step out of yourself. You can apologize. And then the beautiful thing is when you are basically forgiven, or you’re welcomed back into the tribe.
So, that turning toward oneself, turning inward is part of how shame develop. But when we have not state shame or temporary shame or mild shame-- but when we have a trade shame, shame proneness, intense shame, chronic shame – we get stuck in self-absorption. We get stuck in turning in on ourselves. We get stuck in rumination. We get stuck in obsession. This is a direct fruit of the shame experience.
So therefore, when people ruminate in a-- I say, if you’re having obsessive-compulsive disorder or something, and you’re just ruminating all the time, there’s often a shame component because this is just how we’re wired.
Kimberley: Right. It’s so interesting that you say that, and it is. I even know, I can say personally, if I’ve done something wrong, there is sort of a-- I think what you’re saying is the self-absorption isn’t in a critical way. You’re saying it as criticism, it’s more of that you’re just stuck on “Did I, could I, why did I, should have I, why did I do that?” And you’re stuck in that cycle.
Christopher: You get stuck in the cycle. And when we can see the shame in, we can address the shame, then we can get unstuck. And seeing and addressing the shame – so shame is the idea that “I’m bad,” or “I’m incompetent,” or something. We can’t just say, “Oh, no, I’m not bad, I’m good,” because that’s intellectual. That’s in the higher cortical process. It just doesn’t work to try to convince ourselves of something that is so anchored emotionally. So we need to do something really different to address the shame. We need to actually warm up the conversation.
This is what Paul Gilbert figured out back in the year 2000 with compassion-focused therapy, is that you can’t necessarily exchange a critical thought with a positive thought just because you want to, because your attitude has to change, the tone, the way you talk to yourself has to change. you have to warm up the conversation as he says. I think it was just a really profound insight, which is the centerpiece of compassion-focused therapy.
But the bottom line is that when we-- say, if we’re obsessing, and shame is at the root of this, first of all, we need to recognize that it’s the root of it, but then how do we change that loop? We do it by actually learning to be kind to ourselves because we’re obsessing, not as an effort to drive out the obsession or to fix ourselves or to stop this or stop that. We need to just put down our defenses and just say, “Honey, this hurts.” You are suffering and learn to love ourselves as a kind of a wounded or broken person.
I can tell you, in my own personal life, that’s precisely how I got into self-compassion because I had public speaking anxiety, and I was technically an expert in anxiety disorders after I wrote a dissertation on it and so forth. For 20 years, I couldn’t deal with my public speaking anxiety, although I knew everything that one should do about this.
To put it simply, until I learned to love myself as a wounded healer, as a broken person, as somebody who could do nothing about his public speaking anxiety, just to love myself because I had public speaking anxiety, not as a way of driving out the public speaking anxiety. And when that happened, miraculously, I lost my public speaking anxiety. That was like in 2016, after 20 years. I’m sorry, 2006. I, more or less, haven’t had much public speaking anxiety for the last 15 years because self-compassion addressed the shame by warming up my inner experience and embracing myself as a person suffering with anxiety, not trying to do some sort of slick strategy of fixing or overcoming or tricking anxiety out of my system. That didn’t work.
Kimberley: Right. Can you share with us? Because I think that’s such a real-time experience. Can you share with us what that looks like for you? Of course, we can always, in our heads, picture the person who’s presenting and has a lot of anxiety. I think we all know that feeling. What was the shift for you when you were on the stage and then it moved into that? Or did you have to practice it on stage? Can you share a little bit about your experience?
Christopher: Yeah. So I guess, one thing is I’ve been practicing meditation for decades, but I never practice self-compassion meditation. Four months before I had a really important talk, which is that Harvard Medical School, the conference that I had, helped to organize on meditation and psychotherapy. Four months before that, I started to very deliberately practice loving-kindness meditation for myself for the first time in my life. So that meant just saying really nice things to myself over and over again, like, “May you be safe, may you be healthy, may you live with ease,” and things like that. Just over and over, like a mantra. And that became a new voice in my head. It sure was a new voice.
And then when I got on stage at this conference, when I got up the usual terror arose with me, but there was a new voice. So, in these months running up to the conference, I would sit in meditation and I would then think about this conference and I would be horrified, and I would start to panic on my cushion in meditation. But then I would just say really kind things to myself. And as I said, not to drive the fear out, but just because I needed some love because I was such a mess, because I just couldn’t psych out my panic, right?
So, I was just feeling anxiety, loving myself, feeling panicked, loving myself, feeling fear, loving myself. And then when I got on stage, I felt the fear and the love came through. It was like a new voice that said, “Oh, may you be safe. May you be peaceful. May you be happy.” And with that warmth, the anxiety disappears because, I’m sure you’ve heard “Love is the opposite of fear.” It really is because when we can hold ourselves in a loving embrace in the midst of our suffering, it really does downregulate the arousal, the sympathetic stress response. It downregulates the stress response. So, this actually happened all internally without any intention at the time, because I had been building up this habit for a few months. And that was quite amazing.
But I need to say that I don’t want your listeners to think, oh, I just need to do this for four months, and then all my public speaking anxiety has gone or whatever I’m dealing with is gone because I also had what’s called the “gift of desperation.” Now I’m sure a lot of your listeners have that too, which is also known as a “moment of creative hopelessness.”
I was broken. Okay? I was an expert in anxiety disorders. I’ve been meditating for 30 years. I knew everything in the toolbox for anxiety and nothing worked. So basically, I had the gift of desperation. In other words, I couldn’t figure this out. And that’s when compassion is really most effective. Like, what can you do when there’s nothing else you can do?
Kimberley: I resonate with that so much.
Christopher: For example, in medical care, compassion is usually part of palliative care when the doctors have given up on curing you. So then they just try to make you comfortable. But the irony is that in mental health, making yourself comfortable, giving yourself compassion is cure because it downregulates the nervous system. So, if you’re afraid and you find a way to give yourself the kindness and the compassion you need, it creates an entirely different physiology, which is the opposite of fear and anxiety. So, the trick is how to do that.
In my case, what enabled me to do it was that I was desperate. And in my desperation, it finally landed because I was actually simply being kind to myself because there was nothing else to do. Everything else had been tried and failed. I suspect there are a lot of people listening to this talk who know exactly what that means. In other words, you already have the gift of desperation.
My suggestion is, that is a good thing. When you feel desperate like that, that’s when you can really start to warm up your nervous system, warm up your heart. Again, not to fix anything, but simply because you are broken, broken in a good way, broken because you can’t manipulate yourself into a different state of mind. So you have nothing to do, but love yourself, and that will make all the difference.
Kimberley: Right. I resonate with this so much. I have a similar-- not a similar story, but I remember a therapist and I go to therapy. That’s what I do. My clinician, my therapist was saying, “It doesn’t sound like you’re being that kind to yourself.” I’m saying, “No, I am. I am being kind. I’m not saying anything critical.” She’s like, “But it’s how you’re saying it. Like that tone, it’s aggressive. you’re not saying anything so unkind, but it’s so aggressive.” And softening that tone – I had no other choice. I was so frustrated. Like, “What am I doing wrong? I’m not doing anything wrong.” So, that was so powerful for me.
Christopher: One of the sneaky aggressions, Kimberley, is, this is really sneaky aggression, especially for clinicians. And that is most of us have been sort of trained to try to fix things, fix things in ourselves or others. you’re from Australia and there’s a meditation teacher in Australia named Bob Sharples, who talks about the subtle aggression of self-improvement. Actually, in a subtle way, to think I’m anxious and I should no longer be anxious, and therefore I should do this, it seems as if it is compassionate, when actually the most compassionate thing to do is to stop trying to fix ourselves and to be really kind to ourselves because we are broken. That doesn’t mean that you are going to be broken for the rest of your life. What it means is, this is the first opportunity you have to get fixed. That is to say, to get healed by the power of compassion.
So, as Paul Gilbert says, there are three main subsystems in the autonomic nervous system. One is the care system, which we’re trying to activate. The other is the threat system, which is associated with self-criticism. But there’s also a kind of edginess or self-criticism in the drive system. And the drive system is “I’m going to fix this, then my life is going to be awesome.” But if we are hooked by the drive system to try to fix ourselves, we are actually creating obstacles for healing.
Kimberley: And I think that’s so prevalent in this era of social media, and even my clients trying to get into colleges like, “You have to be going and do some much, and I’ll have to be better,” and all these things. I think that’s so true of this era we’re living in. Better, better, more, more.
Christopher: Yeah, that’s right. We’re not very patient. In other words, this is a fast-paced society, particularly with electronics and the internet. But compassion is slow. Compassion is patient. If you think about how do you recognize compassion, there are a number of ways that we recognize compassion. One is with a soft gaze. One is with a soothing or supportive touch. One is with gentle vocalizations. But another way is with patients. When we are around somebody who is not trying to achieve anything, get anywhere, but it’s just with us in an open-hearted way, we know that we’re in the presence of compassion. But how often do we do that with ourselves? Very rarely. When it comes to ourselves, we are usually more impatient than we are with anybody else. And so therefore, we really need to back off. Learn to be with ourselves in a new way. give up the struggle just for a second and see what happens.
Kimberley: Well, that’s so interesting, because if you were to say like, compassion is slow, that is the opposite of anxiety, because anxiety comes with an urgency, right? Like, get away from it. We’ve got to fix it right away and remove it right away. And that is that sort of paradoxical thing of the answer isn’t to run away fast and the answer isn’t to push it away and just to slow down into it, right? Like you were saying, it’s like the give up. It’s like, let’s just stay.
Christopher: When we give up, we’re actually not giving up. We’re just giving up the struggle.
Kimberley: Yeah. Laying down the sword.
Christopher: We’re not giving up. Say it again.
Kimberley: We’re laying down the sword.
Christopher: We’re laying down the sword, right? We’re not giving up that we’re going to have a happier, healthier life. It’s quite the contrary. We’re just doing it in a new way. We’re giving up the struggle and we’re learning to embrace who we are and what we’re feeling in this moment. The great paradox is that then leads to cure. So, it’s a paradoxical cure.
Kimberley: It is. It really, really is. I love this. So, tell me, what are some of the roadblocks you see when it comes to people? I know I’ve done a lot of presentations with you. You do a lot of self-compassion meditations. What are some of the roadblocks you see people go through in trying to access self-compassion? Because for those of you who don’t know, you have created this amazing program called Mindful Self-Compassion. Have you got any kind of reflections on what might be some of the roadblocks?
Christopher: The roadblocks to self-compassion. Yeah. So, there are personal ones, there are more cultural ones. Well, the main roadblock is the term “self-compassion” because when people hear that, they think selfishness, narcissism, not good. Or compassion, they think, oh, soft, fuzzy, I got enough of that, I’m too compassionate already anyway, that sort of thing. So, the term itself is going to be a problem.
And then there are other subproblems such as people associate self-compassion with self-pity, with lack of motivation, with self-indulgence, with, as I said, selfishness, weakness. And all these obstacles to self-compassion are actually myths. There are misconceptions because the research overwhelmingly shows that people who are more self-compassionate are actually more compassionate to others, less self-absorbed, more resilient when things go wrong in their lives, and they are more motivated, not less, more motivated to achieve their goals. They just do it in a different way. They don’t do it with harsh criticism. They achieve their goals through self-encouragement and kindness.
So, those are the obstacles. The research shows the opposite. But people also have individual obstacles, like personal obstacles based on their childhood. So, for example, if we were punished for crying, most males have been told that’s unmanly. So, if I start to practice self-compassion, I might feel vulnerable inside. I might even touch some old wounds that happen. This is called backdraft that love reveals everything, unlike itself.
People recognize that they might have shut down in order to survive. And then when they start to open up with self-compassion, they start to feel vulnerable, maybe some difficulties arise, and then they think, oh shit-- I’m sorry. Something’s going wrong. And that then is an obstacle. But that’s a personal obstacle because it’s related to a person’s personal, let’s say childhood experience.
So, when we practice self-compassion, we need to really understand the territory. We need to know how self-compassion works, what to do when-- so we have a saying: When we give ourselves unconditional love, we discover the conditions under which we were not loved. So, when difficult emotions arise, as they inevitably will, that’s actually an opportunity for healing. But if we don’t know that, that just means, “Oh, I’m not doing this right. Things are not going the way that they’re supposed to go. I should stop.” That’s an obstacle.
So, in this course, this eight-week Self-compassion Training course that Kristin Neff and I developed, now with the help of thousands of teachers around the world, this course actually guides people through the process, such that it is healing. In other words, we learn how to give ourselves compassion. We are open and kind to ourselves when the opposite arises, as it must in order to heal. And then we learn to meet everything that gets stirred up with compassion. We learn to meet that in a new way. In other words, in a compassionate way. And then as a result of that, we actually heal. In other words, we can even reparent ourselves with self-compassion, but we need to understand the territory. Sometimes it’s really good to have a therapist to help you with that.
Kimberley: Yes. I have taken-- just for the listeners, I’ve taken the eight-week course twice, maybe three times, I think. Twice, and then once I think the quick, fast one on the weekend, which I loved all of them. Let me take you back to something you mentioned before, because I want to make sure people are really clear. So, you’d mentioned the shame you experienced because of somebody else’s way they’ve perceived you or that what they’ve told you or how they’ve communicated to you, but then there’s the internal shame. Would you say that the compassion practice is the same for both situations?
Christopher: Well, compassionate, in general, is a powerful resource for regulating our emotions, for coping, for emotional resilience. So, no matter what happens to us, if we know how to be compassionate to ourselves in the midst of that stress, it’s helpful. But I found that there are many things that are helpful when we’re under stress, like getting exercise. But when we’re dealing with shame, then we need self-compassion more than ever because you’re not going to deal with your shame just by, say running a marathon. That’ll calm you down, but it won’t touch your shame.
So, in order to address shame directly, which has these characteristics of self-absorption and isolation, and self-criticism, we actually need to deliver a medicine, which is the opposite. And self-compassion is the opposite. So literally, Kristin Neff’s three-part definition of self-compassion is self-kindness versus self-criticism, a sense of common humanity or connection versus isolation, and mindful awareness versus self-absorption or over-identification.
So, what I experienced, example with my public speaking anxiety, is that I only discovered that I had a shame disorder after I had been giving myself compassion for four months, that in other words, the self-compassion enabled me to finally see what the problem was. It was like a resource or a strength. It was like a platform. It was like a firm foundation that I can actually see what the problem was.
So, when we think about self-compassion as an antidote to shame, we really want to front-load the resource. We want to start getting good at self-compassion, and then we can turn around and touch the shame from a position of strength. And self-compassion targets shame because it’s the opposite of shame. But just let me say that it’s not only the opposite of shame. It has more than non-shame. It is kindness, which is different than non-self-criticism. It has a sense of connection, which is different than non-isolation. It has mindful awareness, loving awareness, which is different than just stopping to ruminate.
So, the cool thing about self-compassion is it has all these positive qualities that actually create positive cycles in our lives. They warm up our experience. They make us happy, which makes other people happy, and it generates a lot of positivity. So, therefore, when we give ourselves self-compassion for shame, we’re not just downregulating shame, but we’re also building a resource, which actually creates – it’s very clear in the research – happiness and life satisfaction.
Kimberley: Yeah. And quality of life, right? Like connection. It is so true. If you talk about shame being about isolating, I think anxiety does that too. It makes you want to hide. But if you can be compassionate, you can stay present with your partner or your child or your best friend or whoever. I think then that is even more healing, right? It’s healing upon healing, upon healing.
Christopher: It’s healing upon healing. That’s a nice way of putting it.
Kimberley: Yeah. So good. Is there something that we haven’t-- I want to be respectful of your time. Is there something that you feel like we haven’t addressed that you want to share on this topic?
Christopher: We covered a lot of ground in this short time. And I guess the main point that we’ve already made, but maybe I can say it again because it’s so critical, and that is, we have what’s called the “central paradox of self-compassion.” And it is that when we suffer, we practice self-compassion not to feel better, but because we feel bad. So, I said this a few different ways already, which I’m pleased about because it is the difference that makes a difference. When we give ourselves compassion for its own sake, it works like a charm. But when we do it as a kind of strategy, some slick strategy for fixing ourselves or how we feel, it really doesn’t work.
So, the metaphor is like, if you have a kid with the flu and your child is crying, “Oh, it hurts mommy. My head hurts. My tummy hurts,” naturally, your heart will go out to the child and you’re not thinking, oh, I’m going to be really nice to my kid so that my kid’s flu will disappear tonight, because it’s a five-day flu. You’re just nice to your kid because you can feel the kid’s pain, right?
Similarly, can we do this for ourselves when we suffer, just like we have the flu? And mind you, we all have the flu. It’s called human suffering and we all do it, and we’re going to suffer until we die. So, this is like a lifetime flu that we all have. And so, what happens when we suffer? Can we be as kind to ourselves in the moment of suffering as we would toward our own child who is suffering? That’s the challenge. When we can do that for its own sake, self-compassion can change your life.
Kimberley: Yeah. Thank you. Oh my gosh, I love it so much. It’s so powerful, and it’s so crucial. I’m so grateful for you sharing all of that wisdom. Actually, we covered double what I was hoping to talk about today. So, I’m thrilled. Share with us where people can find out about you and all your resources. We’ll make sure to have them in the show notes.
Christopher: Yeah. So, we have an organization called the Center for Mindful Self-Compassion that basically is a clearinghouse for everything self-compassion-related training, and you can download audiotapes and videotapes of things. That website is CenterForMSC.org, and my website is ChrisGermer.com.
Also, if people are interested, particularly in the research, you should go to Kristin Neff’s website. She’s really the-- I could say the main pioneer of self-compassion research and she is Self-Compassion.org. Her website is just amazing, and her work is amazing. And she just came out with a book called Fierce Compassion, which tries to correct our misunderstanding that compassion is always soft and tender. Sometimes it’s fierce and it’s tough. Sometimes we need to do really hard things in a kind way. And that book shows people how to do it. So, you can learn more about Kristin at her website as well.
Kimberley: Yeah. She’ll be on the show here in maybe, I’d say six weeks.
Christopher: Okay, great.
Kimberley: Yeah. Again, because she’s been on before. It’s so good. And you said there was a training for clinicians as well.
Christopher: Oh yeah. So, we have a Self-Compassion in Psychotherapy Certificate Program, and this is a 10-- I’m sorry, a 30-week training with a lot of renowned people as faculty. Basically, it teaches how to integrate self-compassion into all aspects of psychotherapy, as well as into our lives personally. It’s a 30-week training, with the first cohorts going to complete the training in the next few months. And there’s a new training that’s starting in October of this year. So, if you’re a clinician and you’re excited about self-compassion and you want to know how do I bring this into my clinical interventions, into therapy relationship, into my own personal life, and into therapeutic presence, that’s the best place to learn it. you can learn about that from that website – CenterForMSC.org.
Kimberley: Wonderful. Well, thank you. I’m so grateful. I have, like I said, such deep respect for you. I’m so grateful for the work. It’s been crucial in the work that I’ve done as a clinician and for myself. So, just major props to you.
Christopher: Thank you so much, Kimberley, and thank you for all the heartfelt and really effective work that you’re doing – getting out insight into new approaches to old problems. Anxiety has been with us since the birth of humanity.
Kimberley: It’s true. It causes a lot of suffering.
Christopher: So, we’ve got a lot to learn, and thank you for being in the center of that conversation.
Kimberley: Thank you.
-----
Please note that this podcast or any other resources from CBTschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day and thank you for supporting CBTschool.com.
Important Links:
https://chrisgermer.com/
https://centerformsc.org/advanced-skills/
Mindful Self-Compassion Workbook
https://www.amazon.com/dp/1462526780/ref=cm_sw_em_r_mt_dp_3YD9C23Q1KQ56WDYCN3C
Mindful Path of Self-Compassion
https://www.amazon.com/gp/product/B005CWSC06/ref=dbs_a_def_rwt_bibl_vppi_i1
This is Your Anxiety Toolkit - Episode 198.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Okay, friends, how are you doing really? How are you doing?
It’s summertime, you guys. Oh my goodness. We’re here. How did this happen? Just to let you know, I will be taking a break as I have done for the last several years over the summer. So I will probably take a few weeks off in July so I can have some time with my kids to really rest and repair and play and be human. It’s such a weird year. And so as I’m recording this, it’s not summer yet, but it’s crazy to think that we’ve landed in summer already of 2021. Am I right? Holy smokes.
Okay, before we get started, as I always say, please do go and leave a review. I will be giving away Beats headphones to one lucky winner when we get a thousand reviews. We’re on our way, guys. So please do go and leave a review. I would so be grateful. It just really helps me strengthen the podcast, and it’s one of my big goals for 2021, is just to really help people with this amazing platform.
All right. So here we go. Today, I am talking about how I am protecting my daughter from an eating disorder. But what I’m really going to be talking about is how we, me and my husband, are protecting my daughter and my son from an eating disorder. The reason I preface that is because, number one, yes, while women are more likely to develop an eating disorder, there is an increase of prevalence of young men and young boys getting and experiencing an eating disorder.
There are many different types of eating disorder. It doesn’t have to be anorexia. They can be binge eating. There’s also types of eating disorders, such as bigorexia, which is around developing muscle. There’s orthorexia. There’s so many kinds of, again, bulimia anorexia, of course, we’ve discussed. There’s so many types and it’s so important that we recognize that this is not just a problem for women and girls.
So let’s talk about it. How myself and my husband are protecting my daughter and my son from an eating disorder. So there are two main things I want to discuss today. Number one is how we talk and number two, how we model. And so I’m going to give you much more detail into how we are doing that and how we’re choosing to do that and the struggles that we’re having.
I, myself, had an eating disorder. So I’m really, really protective of this topic with my children. It’s something I really want to try and protect them from while I know that I can’t entirely protect them. I can do a lot of education to give them everything they need to hopefully not have to go through what I have gone through and what so many people have gone through with eating disorders.
So, first of all, let’s talk about what we talk about. Let’s talk about what we talk about, shall we?
All right. So the first thing, and you guys have heard me say this probably before, the first thing we talk about is diet culture. This is where we identify how our society is teaching us to believe that we should be a certain way. Our bodies should be a certain way. Our skin should be a certain way. Our hair should be a certain way. We should look a certain way. And we want to be able to identify this so we can call the BS on it.
So the reason that I call BS on it is, just because society tells us our body should be a certain way doesn’t mean it’s true. In fact, it’s entirely BS. Your body, my body, my daughter’s body, my son’s body, and my husband’s body – doesn’t have to be any particular way.
Society and diet culture is going to tell us that it should be thin. It’s going to give us all of these messages. “We should be thin. We should be strong. We should be tall. We should be short. We should be eating this certain thing. This product will help us with our metabolism. This product is bad. These foods are good. These foods are bad.” And there’s so many messages that are faulty and proven to be wrong. So, so important. So we talk a lot about this with my children.
When my daughter and I go shopping, which we haven’t done in a long time, but when we see advertisements, when we watch TV shows, when we look in magazines or pitches of books in books, when we look at Barbie dolls, we talk about diet culture. I might say, “What about her body? Let’s talk about Bobby.” And we look at Bobby and I’ll say, “What do you think about her body?” And she’ll be like, “It’s kind of weird. It looks kind of strange.” And I’ll say, “Yeah, why do you think that is?” And she says, “Well her waist is really small.” And I’ll have a conversation with her. We talked to her about, “Do you feel like you need that to be beautiful? No, no, you don’t.”
How might we change this? And I might say to her, “You don’t have to look anything like that. You know that your body is genetically set up to be exactly the way your body is and there’s nothing you need to do any differently about that.” So important.
Same with my son. Look at the action figures. We might say, “Your body doesn’t have to look like that.” That’s diet culture. You don’t have to have a six-pack of abs. He’s only six, but we’re still already having these conversations.
Now, what’s interesting is my husband right now is reading the book to our children, and it was a book that he read when he was a young kid with his parents. It’s interesting because there’s all these references to fat, like fat this and fat boy and fat girl, and she was fat and so forth. We talk about the word “fat.” We talk about, is that a good word or a bad word? No, it’s just a word. It’s a descriptive word. But would we use it to describe somebody else? No. We would use many other things to describe somebody than using that kind of word. Not that there’s anything wrong with the word. It’s just that we don’t want to encourage them to define a person by their body.
We try our hardest not to compliment our children’s body. You might think that’s crazy. Some people go, “Oh, no, no. My child won’t have an eating disorder. I tell them how beautiful they are every day.” I often will educate them and say, “That doesn’t actually prevent anything. In fact, it just adds to that kid and that child thinking that the way they look is important. Because what if their body changes? Then they’re going to be like, ‘Oh no, mom’s always complimenting me on my body, and now my body changed. So does that mean I’m bad?’” So we do our best not to compliment their body or anybody’s body.
I have worked really hard since my own recovery to never congratulate someone for losing weight, which is really hard. In fact, I’ve had one really difficult conversation with our friend where she was saying, “I really just want you to compliment me because I have lost a lot of weight.” And I’ve said to her, “That doesn’t line up with my values. I love you, but I never want to engage in something where you believe your worth is caught up in your body. I just can’t do that. I’m sorry. But I love you and I love everything about you, every part of you, whether your body is in a large body, a small body, a tall body, a short body, whatever color skin. I love you.” And we say the same to the kids. Now, of course, we also don’t ridicule their bodies. We don’t comment on their bodies, their ever-changing bodies, as they, my daughter moves into preadolescence.
We’re still in the talk section. We talk about what we do value. That person is very kind. He has kind eyes. She has a beautiful smile. She radiates love. She is a fun person. She’s very intelligent. My five-year-old son says intelligent a lot. “He is very intelligent. I am very intelligent.” Not that we want to overvalue that either. Because we want to really remind them that unconditionally, we will love them and that their worth is consistent. It doesn’t matter what. It doesn’t matter what. That they’re worth and our love for them is consistent.
And to be honest, I will say there is nothing more powerful than hearing that from a father, particularly if you’re a young woman, a young child like my daughter. For my husband to say, “I love you, no matter what. Don’t ever let a man judge you or comment on your body and you believe what they say, because you’re more than a body.” To teach our son that other girls and other boys are more than a body. To teach him that he’s more than a body. So important.
Now another thing we do is we praise all foods. We celebrate all foods. We are grateful for all foods. We do not have good and bad foods in our family. We don’t talk about things being healthy and unhealthy. While we do very much value health, we really try to help the kids understand that they can listen to their body and our body.
This is the kind of funny story, I’ll tell you. My daughter is going to be 10 and she can outeat anybody. It’s really quite phenomenal. She’s always hungry. And my instinct is to go, “You’ve already eaten. Stop eating. You certainly cannot be hungry.” I’m feeling full and she’s eating double what I have. But I really catch how we talk to her about her food and we celebrate, “Good for you, honey. You’re listening to your body.” She’ll often come to me and say, “Mom, I’m starving. What can I eat?” And we laugh. And she smiles. And I say, “Hun, what do you think I’m going to say?” And she rolls her eyes and she says, “You’re going to say, ‘You can eat whatever you want.’”
Now, of course, we have some rules around this. We don’t encourage and we don’t allow the kids to eat a lot of snacks before a meal. We try to really have them understand the importance of waiting for their meal. But that’s probably 45 minutes at the most. Often my daughter will have a full peanut butter and jelly sandwich 45 minutes before a meal and still eat her whole meal, and we praise her for that.
My son is really, really picky around food. There’s certain things he really, really likes. And interestingly, he has no interest in sweets. If he could choose between salty and a birthday cake, he would choose salty all the time. We encourage him to just listen to his body. I talk to them about me listening to my body. They’ll be like, “Mom let’s go have ice cream.” And I’ll usually sometimes not eat ice cream. That’s not because I’m restricting. I might say, “No, I’m listening to my body. I don’t really need ice cream right now.” And then there’s other days where I’m ordering three scoops of ice cream because I’m really hunkering down for some ice cream. So I try to also teach them that it’s okay to listen to your body as does my husband.
So these are all really, really important things we talk a lot about. And this is the last thing we talk about, which is health. What is health? Is health only eating sugar-free foods? Is health being thin? Is health being tall? No, none of those things. Is healthy eating only organic food? No, absolutely not.
Health is having balance and taking away judgment. We have to remember here too, health is not just physical, it’s mental.
I know people who eat the most “clean diet” and they exercise, but they’re not healthy because emotionally they’ve got a really unhealthy relationship with food and their body. They’re hard on themselves. They beat themselves up. Maybe they binge. So this is the thing to remember. Your definition of health might not be what is the real definition of health.
Now this is really true and I’m going to make sure I have some people on coming here once we get back after the summer on talking about health at every size. This is a crucial conversation we need to have. If you haven’t read yet a book called Health at Every Size, I urge you to. It’s so important to really understand the science behind that and understand the issues we have around how we have stigmatized people in bigger bodies as being unhealthy when we’ve actually got lots of science to prove that you can be really healthy in any size body, that health is not indicated by just your size.
Okay. So now we move on to what we model. This is similar, but very important. So my husband and I have two completely different body sizes. Not that that’s super important, but I feel it’s important for our children to have those two examples and to have family members with different body sizes, where we celebrate every single body, and we do a lot of modeling around that. We do a lot of modeling, celebrating bodies – all the body sizes, shapes, skin colors, nationalities, sexualities. We try to model to our children and normalize differences instead of things being like, “This is good and this is bad.”
We also model, like I’ve mentioned to you, how we eat. We try not to judge each other for what we eat in front of each other. We try to really encourage by modeling like there’s no time you should eat food. A lot of my patients will say like, “Oh, I had a bagel for breakfast so I can’t have a bagel for snack.” And we go, “No, you can eat a bagel for breakfast and for lunch if you want.”
My son loves more than anything to put cream cheese and sprinkles on his bagels in the morning. He loves really sprinkled-up bagels and we allow it. We figured it’s no different than him putting jelly or jam on his bagel. And so we allow it, we allow him to enjoy his food. Given that he’s a kid who doesn’t like a lot of sweets, we’re all for it.
We also model by not saying negative things about our own body. My son is a personal story, but my son once came in and I was getting out of the shower and he said, “Mom, your belly’s all jiggly,” which is most moms’ nightmare. You know what I said? I said, “Yeah, it is. Isn’t it beautiful though, that I had two babies in that belly? Isn’t that cool?” He might say, “Daddy’s belly is big,” or whatever he may say. And we’ll go, “Yeah, isn’t that wonderful? We have so much fun eating food and what a wonderful body. Isn’t it so great that we have our bodies, that our bodies do all these things for us, like pump blood and breathe and digest food and run and hold our hearts and hold our brains and filter nutrients and things like that? Isn’t that incredible?” We model body acceptance and body love.
This has been really helpful for us, particularly because I know a lot of women and men who’ve developed eating disorders because their parents were on a diet all the time, that their parents model these strict diet culture rules, and good and bad rules, and all of this stuff that’s so dangerous for young ears to hear.
Now, we also model this or share one more personal story is, so much of eating disorders is around restriction. Over the last two years, my daughter has had some medical issues where she had to restrict several different food groups and this was really uncomfortable for me. I was very strong against it. I had said to her pediatrician, “I’m very uncomfortable with this. I do not like the idea of her restricting.” And he really coached me through. “You have everything you need to help her protect against this becoming something eating disordered. And just because she needs to do this medically doesn’t mean we have to make it about her body,” which was really helpful for me to hear. And so, yes, she has had to restrict several really important food groups because of some stomach issues that she was having.
And so it’s been a really interesting thing for us to have these conversations around what is a diet and what does that mean and why would we go on a diet and what are some reasons that we probably would not encourage her to go on a diet around and so forth. And so, that has been really, really fascinating to watch her navigate that.
There’s been a couple of times where she said like, “Mommy, I know I’m supposed to check on the ingredient list for certain things.” But she said, “That has made me really uncomfortable having to do that.” And I so appreciated her talking to me about that. And so we came up with basically a strategy that she could know basically what is in certain different foods. And from there, she wouldn’t have to look at the nutrient lists anymore, the ingredient lists. I was so happy that she felt comfortable saying, “This feels not right for me. This feels like it could become a problem.” And so, that has been really, really huge.
I think the only thing I would add from there is, for me as a therapist, but mostly a mom, I’ve had to really allow a lot of space for anxiety around this stuff because I never want my child to have to go through that. I have caught myself being hard on myself and feeling a sense of hyper responsibility, like it’s your job, it’s your job to protect her. I’ve had to really pull back on that as per my conversations with the pediatrician in terms of saying, “Kimberley, you can do what you can do, but you don’t have control. It will be what it will be. You can model and you can talk and you can be the best you can be, but we also have to let go of control and just be uncertain.”
Like I’m always telling you guys, it’s an uncertain thing. There’s no promises that we can do the best that we can. If we make a mistake and we mess up, we apologize and we share and we talk about where that mistake in that era came from, where did we learn it, what triggered us in that moment. And so, that has been really, really important for me as well.
So I hope that that’s being helpful. Those are the main pieces that have helped us as a family to protect our daughter and our son from an eating disorder and body image issues. I do hope that even one point has helped you in navigating this.
If you haven’t, if you’re not the parent of somebody, these are also messages and things that you’ll have to do for yourself, to model to yourself, talk to yourself about. And if not, go and find an eating disorder specialist who can help challenge this and work through the beliefs you have around food and diet culture in your body, and that can be really, really, really helpful.
Okay. I love you all. Have a wonderful, wonderful day. It is a beautiful day to do the really, really hard thing and you’re doing it. I know you are. So, I will talk to you very, very soon.
Have a wonderful, wonderful day.
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 197.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
 Welcome back, you guys. So grateful to have this precious time with you. Thank you so much for coming and spending your very, very precious time with me. As we do this together, it’s exciting, we’re almost at 200 episodes. You guys, I cannot believe it. I am pretty, pretty proud of that, I’m not going to lie.
Welcome back, you guys. So grateful to have this precious time with you. Thank you so much for coming and spending your very, very precious time with me. As we do this together, it’s exciting, we’re almost at 200 episodes. You guys, I cannot believe it. I am pretty, pretty proud of that, I’m not going to lie.
Today’s episode is with the amazing Jon Hershfield. He’s been on the show multiple times and I have been really reflecting and thinking about how important it is for us to practice response prevention and how that is so, so important for everybody who has any type of anxiety, whether that be an anxiety disorder like OCD, social anxiety, specific phobia, generalized anxiety. Even for myself, I’ve been reflecting on any time I’m responding to fear and responding to discomfort. It’s just a topic that I want to continue to address because I think from you guys, I just continue to see how much it’s a struggle for you.
As I thought about continuing education on tools you can use, I thought, who else can I have none other, but Jon Hershfield to talk about using mindfulness to manage compulsions. Now we talk about compulsions like mental compulsions and rumination. We talk about reassurance-seeking, avoidance, any kind of physical compulsion. We also talk about how to practice mindfulness so that it doesn’t become a compulsion. And so I’m just so grateful to have John give us his very valuable time and to talk with you guys about these amazing concepts.
I’m not going to spend too much more time doing the introduction. You guys know how amazing Jon Hershfield is. He has some amazing books. He has The Mindfulness Workbook for OCD, and he has Everyday Mindfulness that he co-authored with Shala Nicely, and The Teen OCD Workbook, and Harm OCD book. He’s just written amazing books. So please do go out and support him. He does share all that information at the end of the show, and I can’t wait for you guys to listen.
In the meantime, please do go and leave a review. It helps us to reach more people. I’m going to be quiet now and let you listen to Jon’s wisdom. Have a wonderful day.
-----
Kimberley: All right, welcome. I am so happy to have the amazing Jon Hershfield with us again today.
Jon: Thanks for having me. You make me sound like Spiderman of the OCD world.
Kimberley: You are the Spiderman of the OCD world. I love it.
Jon: What does that mean?
Kimberley: Yeah, it’s true. Well, that’s a good thing. I know my son is probably jumping up and down at the idea of me meeting the Spiderman of something. Thank you for coming on. I really wanted to invite you on, of course, because I love the work that you’re doing regarding mindfulness in OCD. I really wanted to talk about how we can use mindfulness, particularly to address compulsion, because a big part of Exposure and Response Prevention is the response prevention piece. I would really love to pick your mind on how you implement mindfulness as a part of that and also address some of the misunderstandings that happen regarding mindfulness.
So, let me first ask you, just for those who don’t know or new to the show, how would you give a definition? How would you explain mindfulness, particularly in the respect of treatment?
Jon: It’s interesting because we all make this same grammatical error. I do it too. We say we use mindfulness as if mindfulness was an act or an action or a thing that you use as opposed to a perspective that you take. So I’m thinking about what mindfulness means. Usually, the definition we hear is “Paying attention to the present moment as it is without judgment and without the desire to change it.” And that’s a great definition. It’s escaping me at the moment who actually coined that exact language, but I think it applies to most mindfulness concepts.
But I don’t like that it starts with the word “paying” because it still implies that you’re doing something. I think mindfulness is actually the perspective that you have when you’re paying attention to the present moment. If you want to play around with the words, it’s really noticing the fullness of the mind – mindfulness, right? It’s a position that you take as opposed to a thing that you do. Right now, I’m sitting here in my desk chair. I’m aware of the sensation of my body in the chair, hearing my voice in the headphones and I have coffee and tasting that coffee. These are all things that I’m noticing and I’m being mindful of.
The other part of mindfulness that I think is important to understand is that, in a state of mindfulness, you’re best able to observe the difference between an experience – I just listed for you a bunch of experiences – and a story. A story is a narrative. It’s the meaning and the webs that we weave around those experiences. So it’s me thinking I’d had too much coffee today, right? That’s a story about the taste of coffee in my mouth right now and its significance, but they’re two separate things.
When we’re treating something like OCD, which is very much about being pulled away by your mind into these narratives, these fear-based narratives – to be able to drop out of the narrative and into the experience would be to take a mindful perspective, or in colloquial terms “to use mindfulness.” But I think a lot of times when we say “using mindfulness,” we associate that with stopping what we’re doing and focusing on the breath, or pulling out an app and doing a meditation, or trying to execute change in our environment by being mindful. When in fact, mindfulness is very much the opposite of that. It’s not about executing change. It’s actually about stepping back and seeing the way things really are.
Kimberley: Right. I love this. So would you say in this perspective that mindfulness is not adding something on, it’s just dropping down into what was already there?
Jon: Yes. I would agree with that.
Kimberley: I like that. So how might we use this, particularly in terms of managing anxiety or uncertainty or any other discomfort? Can you give me a walk-through of what that might sound like or look like for somebody who is practicing mindfulness?
Jon: Well, one of the things you might think about, when somebody feels triggered, something happens. You’ve touched something you think is contaminated or you’ve become aware of an unwanted, intrusive thought, a harming thought, or something like that. Then you have an experience in the brain and in the body that alerts you to the fact that you’re under attack, that you’re distressed, something is wrong and it needs to be fixed.
What most people do is they immediately go into the story of, “This is bad. I’m triggered. I need to get away from this trigger. How do I make this feeling go away? Because it’s unpleasant.” Of course, it’s unpleasant because it’s your brain’s way of trying to help you jump into action to get away from the things that could harm you. So it’s natural that we want to get rid of this feeling.
And then we do these things called compulsions that reliably, in the short term, get rid of these feelings. If you know anything about OCD as you do, it’s like you get stuck in that loop. The more you compulse, the more you really feel the responsibility towards your obsessions as they arise.
In that space, between the trigger and the compulsion, there’s an experience you’re having. A person who has been practicing mindfulness or who is mindfully aware can show up to that experience in the same way they might show up to other experiences, again, without having to make it go away. So you render the compulsion less important because you’re willing to be in the presence of that triggering experience.
If you were to take this to the mat and think about, “Well, what happens when you’re meditating and you get an itch?” what is the instruction? It’s not, “Well, just scratch it so you can be more comfortable.” It’s usually, “Okay, well, notice what itching is like. Notice what it’s like to be sitting, which is what you’re doing, and then have your attention pulled away from the sitting to the sensation of itching, to be able to say, ‘Oh, that’s itching.’”
Now at some point, we all break and we start scratching ourselves all over it because it’s too much, but that’s fine. But that’s not the first instruction. The first instruction is simply notice itching. And then if you’re capable of letting go of that and going back to what you were doing before you got distracted by the itch, you’d go back to your breath or whatever the anchor of your meditation might’ve been.
It’s the same thing in real life. You’re minding your own business. You’re trying to read a book and then you have an intrusive thought that something terrible is going to happen. And then you notice that experience of this mental itching and you’re, “Okay, that’s happening.” And then you have a choice. You can drop down out of that back into your book, or you can dwell on it, ruminate on it, try to figure it out, try to figure out a way to make it go away, and then give yourself permission to go back to your book.
Kimberley: So, we call it in my practice, my staff have called it “itch surfing.”
Jon: Itch surfing. Yeah.
Kimberley: I always laugh when I say “itch surfing.” So, let’s say you have the presence of a thought that’s really concerning, right? It’s triggering. And you’re trying to be mindful, but you’re also not trying to step across the line to where you are ruminating or being compulsive related to that. How might someone differentiate between the two?
Jon: So there’s a couple of things to consider here. One is that a lot of people will say, mindfulness is about watching your thoughts come and go. There’s a good reason why we use that metaphor, that idea of sitting at the bank of the stream and watching the leaves go by. But it’s not really accurate in the sense that it’s more about just noticing thoughts coming and going. Watching thoughts coming and going implies that you’re supposed to sit there and stare at them and give them special attention. You’re supposed to remember, right? It’s a perspective. It’s not an act. You’re supposed to remember like, “Oh yeah, it was a thought coming and going. Okay, that’s cool.” And then let go of it.
Ruminating is when you’re digging up that thought for the purpose of trying to figure it out to digest it. You’re trying to act on the thought and get certainty about it. It’s a very active thing you’re doing when you’re ruminating.
To be mindful would really be the opposite of that. It would be to notice that you’re ruminating and stop. Because the whole point, if you’re being mindful, it’s not that you’re executing change on your environment, but you’re simply noticing what’s coming up. So it was really impossible to be mindful and ruminate at the same time because that would be like being mindful while trying to figure out some problem.
So the instruction would be to notice that urge to ruminate, to notice what’s coming up for you in your body, that experience of, “I really want to figure this out,” and then to allow that experience to be there, and again, drop back down into your anchor. In real life, it’s whatever you were doing before you got distracted. In meditation, it’s whatever your anchor is – the breath, the feeling of your body in the seat.
Kimberley: So it’d be like using the metaphor of, if you’re sitting at the edge of the stream and you’re just watching the leaves come and go, that would be mindfulness. But ruminating or being hyper-aware would be like watching the leaf after it’s way, way, way, way down the river, but you’re still giving that attention and missing what’s right in front of you?
Jon: Yeah. It’s easy to make that mistake because you could feel like you’re being mindful. You could say like, “Well, I’m just watching this leaf and seeing how far it goes.” But in fact, when you’re doing that, you’re missing everything that’s happening in the present moment, all those other leaves that are going by.
A lot of times, people think of themselves as being very negative because they get distracted by negative thoughts, and the thought comes down the stream and they follow it. And while they’re falling, those negative thoughts, all sorts of other nice things are happening – the smell of their breakfast or the warmth of the sun or whatever it might be. But they’re not noticing that stuff because they’re immersed in tracking that negative experience that they had. They think of their lives as being negative instead of thinking of their lives as just being whatever it happens to be in any given moment.
Kimberley: Right. Talk about, if you will, hyper-awareness, because I think sometimes people think they’re being mindful, and I think it’s going to be very similar maybe in your answer, but I just want to be really clear for people who I’ve heard struggle with. They’re trying to be mindful, but it becomes hyper-awareness. Do you have any thoughts on that?
Jon: A lot of this, I think, comes down again to language. Most of us are trained to say things like “Sit with uncertainty,” which sounds like a good idea, but the implication for some is that you’re literally sitting and there’s literally uncertainty in front of you. It’s like sitting on your head and you’re immersed in it and you’re dwelling on it. So it gets translated as “Dwell on uncertainty,” and feel bad as long as you can feel bad.
Actually, I interviewed Jon Abramowitz who some of you may know in a lecture series here at Sheppard Pratt not too long ago. He said he likes to say, “Act with uncertainty instead.” I really like that because to me, that is still mindfulness. You’re doing something, you notice you became distracted, cool. That’s what that’s like. Now I’m going to go back to what I was doing before I got distracted. I’m going to act with the uncertainty instead of sitting, letting the uncertainty sit on my head.
I think it’s such an important distinction because to be mindful of your thought process is to be aware of it. But it’s not the same thing as to be trying to figure it out or be certain about it. That would be the opposite of mindfulness. And so the whole instruction, if you’ve had a lot of experience meditating, it might sound something like you wander away from your anchor and you start trying to figure out what’s wrong with your life. And then you go, “Oh yeah, thinking.” And then you go back to your anchor. No meditation teacher is going to tell you like, “Well, just notice that you’re trying to figure it out and keep trying to figure it out and try to get to some sort of outcome.” That really would go against the larger project.
Kimberley: Yeah. I mean, for me, if I were to explain it, if I were out and about, and let’s say another emotion showed up, like shame or guilt or something, my practice is just to go, “Oh, hi, Shame.” I think actually in the last episode, you were here talking about teens and you were like, “That’s cool, bruh,” or whatever it was, but that’s observing it and allowing it to be there. But then there’s a redirect to the present. Would you agree that’s a method that you use? I mean, again, we’re saying it’s not a doing, but talk to me about whether that’s something that you would apply to.
Jon: I would absolutely apply that. I mean, at the end of the day, we’re coming up with fancier and fancier ways of politely and compassionately saying, “Let it go.” We might have all the different ways of saying “It’s okay to let it go,” where we understand that it’s very painful to have these experiences and that makes it difficult to let it go. We don’t mean let it go, like, “Oh, you’re being silly.” I mean literally, it arrived and you allowed that, and now it’s leaving and you can allow that to let it go.
To become aware that you have an urge to ruminate or an urge to do some other compulsion and to let that urge be a thing, don’t sit there and stare at the urge and wait for it to go away. just be like, “Oh, that’s happening.” Just like shame arises or guilt arises. And then just gently note it and allow it to be, and you don’t have to do anything. It’s really a beautiful thing. The shame and the guilt and the urge to ruminate and the urge to wash, it’ll go away in its own time. You don’t have to be actively involved in it.
Kimberley: Right. It’s like mindfulness underneath there. A major component is non-attachment, to not be attached to it or the story we tell about it or what it means and all the things.
Jon: I mean, if you look at that and the concept of diffusion, they have specific skills for trying to make that happen. I think people can argue over like, “Well, what are the mechanics of building those skills? And could there be some compulsivity involved in that?” I mean, I think there’s some people that certainly could. If you’re going around saying, “It’s just the thought, it’s just the thought, it’s just the thought,” that’s not exactly what we’re getting at when we talk about diffusion. But the end game is diffusion, it’s being able to say, “I’m having a thought that...” What we want is to be able to do that without having to say it, without having to remind ourselves. But instead, simply have the experience that the thought arises much the same way the credits in a movie arise on a screen. Okay, yeah, that is the thought.
And then you get to decide, “Do I want to engage with this or let it go?” If it’s an obsessive thought that you’ve been grappling with, that you’ve decided is your OCD because you keep trying to get certainty about it, well then the instruction is going to be to drop it, not to play with it.
Kimberley: Right. Yeah. I think that this was a lesson for me early in my mindfulness game. Mindfulness is not just that heady, heady meaning like only a cognitive skill. It’s like you talk about dropping down, and it’s a behavioral skill as well. It’s not just sitting still and thinking, thinking, thinking, thinking your way out of discomfort. It’s also a doing. It’s a body thing as well, instead of it just being heady. I think that’s where we get into trouble, right? We start to try to think our way out of problems or our way out of discomfort.
Jon: Look at checking OCD, for example, like OCD where there’s a lot of checking compulsions. What happens is there’s this experience of not being complete, something missing or something being lost. And rather than own that experience and be able to say, “That’s something that just came up for me and I’m willing to allow that,” the instinct is to get rid of that experience by engaging in the checking compulsion. So, mindfulness plays an important role in being able to say, “I’m aware of this urge to check, and that’s fine. I have all kinds of urges throughout the day. I don’t have to give in to this urge.” You don’t have to do anything about it.
Like you were saying, that’s an experience you have in the body, like a sense that the body is craving a change and your willingness to allow that craving. Again, not to sit there and stare at it and wait for it to go away, but just simply just know that it is there and then go onto the next thing.
Kimberley: Right. I think that this is true in so many compulsions. Would you use the same skill? Would you use the same concepts regarding reassurance-seeking compulsions?
Jon: Yeah. Well, reassurance-seeking is really just another form of checking, isn’t it? It’s like you have a sense that you know something, just like you have a sense that your door is locked when you go back to make sure. In the case of reassurance-seeking, you’re going to a person or the internet to try to make sure. But again, it’s that experience of dis-ease, right? Not feeling ease with your experience and wanting to change. Instead of resisting that by doing compulsions, you’re saying, “I’ll allow it.”
I’ve been using this coping skill with the client. I might have mentioned that they prefer “allow” rather than “accept” because accept felt, I don’t know, it felt different to them. We can use whatever language you want, but I liked it. I’ve noticed that as a coping statement. If something comes up, like, “I want to change it,” and they’re like, “Nope, I’ll allow it.” And then now you’re free.
Kimberley: Open the gates to it.
Jon: Yeah.
Kimberley: Right. I like that a lot. The same goes for avoidance, right? Do you want to share how you might drop into mindfulness when it comes to avoiding, whether you’re about to avoid or you’re already in avoidance? What would your thoughts be there?
Jon: Well, it’s like observing your inner magnet, right? Something is pulling you in a direction. It might be pulling you away from something or pulling you towards it. And again, what does that feel like for you? What does that experience in the body? And rather than telling yourself “Accept it, accept it, I got to accept it, and push, push, push, push, push,” can you just notice where the resistance is? Can you let go of that, that part of you that’s resisting? you want to go to this party, but it’s overstimulating and you might say something embarrassing and there’s something there that might be triggering for you or something like that. But you want to go. As you’re approaching it, do you notice that resistance? Do you notice that push-pull in your body? And again, can you allow it? Can you say, “Worth it, investment return, worth it.” Very quickly, not spending a lot of time on it.
Again, I think cognitive therapy gets a bad rap a little bit in the OCD world because it can so easily turn into mental rituals, trying to assess the probabilities and things like that. But just a pinch, like a pinch of salt, a pinch of cognitive therapy where you’re able to say, “Come on now, this is a black and white thinking. I can handle this.” If you’re allowed to do that.
Kimberley: It’s funny that you say that because I was actually just about to ask you, like, go back to your story. Remember at the beginning, you were talking about the stories we tell ourselves. And I think in avoidance, there are so many stories that take us away from mindfulness. So I was actually going to ask you. Do you want to share how you would maybe implement a cognitive skill there?
Jon: So, if you’re being mindful, it means that you’re aware that you’re thinking. And if you can be aware that you’re thinking, you can also be aware of the tone of thinking. This is especially useful if you’re trying to quickly assess. Are you ruminating? Are you engaged in mental rehearsal? Are you thought-neutralizing? What is the mental behavior? If you’re noticing the way that you’re thinking and that tone, you might be able to pick up historically if that tone has been helpful or not, or if it usually ends in you feeling like you have to do compulsions.
Take catastrophizing, for example. You’re saying, “Something in the future is definitely going to go badly and I’m not going to be able to handle it.” Now, if you’re aware and you’re mindful, you know you’re thinking, and then you know that that’s what you’re thinking, and you know that that’s catastrophizing, you can simply say, “Yeah, that’s catastrophizing. I don’t need to do that right now.” Very simple. “I can’t predict the future.” You don’t have to go into “Everything will be fine,” or “The probability is that this is going to go my way.” Again, we want to spend as little time there as possible because we don’t want to get wrapped up in arguing with the OCD, but to just call it out and say like, “I can’t predict the future. I’m going to just go with this and see what happens.” And then when you make that choice, notice what that feels like. Can you allow that or not? And if you can’t, that’s okay. You can go find something else that you can allow.
Kimberley: Right. I will always remember many, many years ago, probably even when we worked together, a client of mine, and they gave me permission to tell this story, but I won’t, of course, disclose any information. But they always said they can feel the shift in their body. And that was them being mindful. They said as if they were holding onto the sides of their chair. So even though they weren’t sitting in a chair, they could feel this shift in their body of clenching. You can’t see me on the video. You can see me on the video, but listeners can’t. But just this wringing of the hands or clinging of the hands, and that her being able to just identify that slight shift in her body was enough to be able to shift out of that avoidance or resistance. I think just being aware and mindful of that, I think, is a big piece of the pie.
Jon: So, it’s knowing the quality and the tone and the texture of your internal experience. That’s essential for being able to pick out and resist mental compulsions. Ruminating is not just thinking about something because you like to think about it. Ruminating is very much like, there’s a puzzle and you’ve put all the pieces together but one, and now you can’t find that one piece that it’s somewhere. Maybe it’s on the floor, it’s under your desk. You know what that feeling is like. It’s so intense. And that mental quality is what’s going on with the person who’s ruminating. And that’s what they have to let go of, or be able to experience to let go of the ruminating.
If you can’t truly appreciate the tone and texture of your mind that “Sometimes when I’m thinking this way, it feels like this, sometimes when I’m thinking this way, it feels like that,” it’s just very difficult to trust yourself enough to call out the mental compulsion as they happen.
Kimberley: Yeah. I love this so much. I think it’s so important that we do address it. So, in all, I know there has-- we have addressed this, but I want to make sure we’re really clear. Do you believe that someone can mindfully ruminate?
Jon: I think it’s an oxymoron because to be mindful is to remember that everything going on inside is an object of attention, and to ruminate is to really engage in a changed behavior. So it’s really the opposite of mindfulness. There are types of meditations like traditional meditation. You have an anchor. You notice when you’re not paying attention to the anchor, you return your attention. Then there’s other types of meditations that might involve free-floating, like free-associating. Notice that this thought then connected to that thought, then connected to that thought. That is a kind of meditation. And you could argue that there’s a kind of mindful awareness of where things are going when you’re doing that. I still wouldn’t call that ruminating though, because ruminating is done with purpose. It’s done with a specific intention. It’s not just watching where your thoughts land.
Now, if you have OCD and you’re learning to meditate, I certainly wouldn’t recommend you do the type of meditation where you just watch your thoughts bounce around each other. But if you’re a more experienced meditator and you want to do that free-associating of watching each thought arise and fall and rise and fall and connect to other thoughts and feelings, that can be fun. But it’s not ruminating. To ruminate would be to intentionally try to figure out or try to get certain about your obsessive content. And I don’t think that there’s any mindful way to do that because it is literally the antithesis of mindfulness, in my opinion.
Kimberley: Right. No, and that’s how I was trained on it as well. I think the thing that I often will say to clients is, anything can become compulsive. Treatment can become compulsive. If you were to technically look at the term, engaging in compulsive treatment isn’t actual treatment because it’s going in the direction of doing compulsions, which is not the technical term for treatment.
Jon: It’s tricky with exposures. For example, I encounter people all the time who are doing checking compulsions but calling them exposures. “I have a fear of something. So I’m going to go over and pretend to do that thing and expose myself to that fear by being in this scary situation. And then it’s going to go away and then I’ll know that I’m not going to do that thing.” Well, that wasn’t an exposure. It might’ve been hard, but it really wasn’t ERP. I usually tell people not to do ERP when they want to. That’s usually suspicious of that. And also to consider what the point of it is. Like, if your OCD is getting between you and some valued behavior, that’s a good reason to go do that ERP. But if it’s not, and it just exists in your head, you don’t have to go ahead and be ready to go find any ERP to do. You’re allowed to just live your life. That’s allowed.
Kimberley: Right.
Jon: Yeah. I think that the other thing that happens with rumination that I think is very confusing and hard for people to appreciate is that, though, I wouldn’t say you can mindfully ruminate. You can certainly be lost in thought and you can certainly ruminate without full awareness of what you’re doing, because a lot of it is habit, right? Rumination, some compulsions, they can become habitual, but most of them are pretty easy to tease apart from habits. But mental behavior is a little bit trickier, I think.
In the same way that a person who’s-- let’s say they have difficulty with biting their nails, and they always bite their nails when in front of the computer. The computer becomes the cue to bite their nails. The hands go up to their face. They start chewing on their nails. They’re not necessarily thinking, “Oh, I’m going to bite my nails now.” It’s just happening. And then they might become aware of it. And if they’re working on it, then they might use a habit blocker or some other strategy that they might remember to be mindful of the urge to bite it and come up with another strategy.
The same thing happens in the mind where if you’re someone who’s used to engaging in compulsive rumination in different contexts of your life, there are going to be things that actually cue you to do it without you paying attention. You might not notice that, but it’s like, “Oh, every time I’m in this chair, I start to ruminate.”
The goal here in terms of improving your mental health situation would be to take ownership of the moment that you become aware of what you’re doing. Not to beat yourself up for ruminating, because again, your mind was like, “Oh, are we sitting in that chair? Okay, sure. Let’s bring up that topic and start reviewing it.” And you can’t take responsibility for something you can’t control.
You might argue, “Okay, well, that’s not really rumination because you’re not the one trying to control it,” but it has all the same words. You’re just lost in this thought of like, “Well, I know this thought must not be true because of this and that, plus my therapist said this and I read in a book, blah, blah, blah, blah.” You don’t know that you’ve left the building. You still think you’re sitting in the chair. But then, boom, you become aware. You suddenly remember, “Wait a minute, I’m a guy sitting in a chair, having a thought, and wait, I’m trying to figure out if my obsessions are true. Nope. Not going to do that. That’s rumination. Okay, good. Where was I?” Let it go.
But I think people can get very self-critical, really hard on themselves, and say, “I can’t stop thinking, I can’t stop ruminating.” In part, some of that is then taking responsibility for something that’s-- it’s just habit. It’s just the brain has been trained to just start revving up the engine. That’s all right. You’ll catch it earlier and earlier and earlier if you practice.
Kimberley: Right. Okay. Is there anything else that you feel we haven’t covered in this area? I mean, of course, we haven’t covered everything, but is there anything that you really want to drive home here in this conversation?
Jon: Well, I guess one thing that’s been on my mind is, we talk a lot about how thoughts aren’t the problem, right? If you’re being mindful, thought as a thought is a thought. And if you have mastery over your OCD, whatever, a thought about what day it is or a thought about hurting your baby, they’re just thoughts. It’s no big deal. And to some extent, that’s true. We don’t treat OCD by treating what thoughts people have. We address how they’re relating to those thoughts and what behaviors they’re choosing in response to that experience.
But in the interest of remembering self-compassion too, I think it’s important to recognize that it may also be the case that people with OCD are more predisposed to the average person to receive certain types of thoughts in a certain way. So even though those thoughts are normal events, it is normal for you to have thoughts about all of the potentials in human existence, all of the different things. We can kill and have sex with all of these things. It’s totally normal to have thoughts about them. But it might also be that when you have that thought, it hits you in a way that immediately generates an urge or a moral responsibility to address it.
And yes, mindfulness can help because it can help. You both recognize the arising of the thought as an object of consciousness and the arising of that desire to do something about it as an object of consciousness. But it’s also worth noting that it’s just hard to have OCD sometimes. And every once in a while, you’re just going to get sucker-punched by it. And that’s not because you’ve done something wrong, it’s because your brain is conditioned or wired to receive some thoughts in that way. And that can be something that you develop mastery over. But I think when we take all of the emphasis on behavior and none of the emphasis on perspective or predisposition, some people feel like they’re not being heard.
Kimberley: Yeah. Thank you for saying that. I think that that’s been largely the feedback I have gotten as well. If people are struggling and they don’t want to struggle, and they’re trying to navigate this thing, that feels like an absolutely crazy puzzle that, like you said, they don’t even have all the pieces. They don’t even have half the pieces yet. So I totally really loved that you said that. I love the idea of compassionate responsibility, which is, we can take responsibility for our experience with the absence of self-criticism. I think we sometimes think that owning this and experiencing this has to mean you have to beat yourself up and that it has to be like “You should’ve done better” kind of thing. But I do not like that.
Jon: Well, you’ve recently written a book on the subject, and I could go on and on about self-compassion. We could do a whole other episode on it. But I do want to end on this note, which is, a lot of what mindfulness means is simply being honest, and we often lie to ourselves about our experiences. We say, “I should have known better,” but when you look at it, there’s no way to have known better, that everything you’ve done is preceded by a thought or an urge or an emotion and we can track this back very, very far. I’m not making the case for no free will or not taking responsibility for anything. I’m just saying self-criticism is inherently dishonest. I say, “I’m a bad person.” That’s a story. That’s not an objective fact. I say, “I feel terrible.” That’s an experience. That’s honest and that’s also mindful.
Kimberley: Right. I love it. Thank you so much. I’m so grateful. I wanted to navigate all this, but I didn’t want to do it on my own. So, thank you for coming on and helping me because you’re just so good at explaining this stuff, and I really appreciate the way that you conceptualize this. So thank you.
Jon: Well, I appreciate you inviting me. I always love hanging out.
Kimberley: Yeah. Are there any projects or things you’ve got going on that you want to share with us?
Jon: Well, right now, we’re working really hard at The Center for OCD and Anxiety at Sheppard Pratt. We have some new team members and so we’re helping a lot of people that way. Not too long ago, we launched the residential program, the OCD program at the retreat here at Sheppard. We’ve had a few people come in and out of that program. It’s really exciting because it’s just a different way of working, working as a team on one or two cases at a time and seeing them every day. That dynamic is new and exciting for us. And then book-wise, the OCD Workbook for Teens is out there. The second edition of Mindfulness Workbook for OCD is out there. I just started working on a new one that I’m co-writing with a friend on how to combine ERP and DBT.
Kimberley: That’s fantastic.
Jon: Yeah. So, dealing with relentless thoughts and painful emotions.
Kimberley: Nice. That would be so important.
Jon: Yeah, I hope so.
Kimberley: Oh, without a doubt, DBT is such an important piece of the work, particularly when those emotions are really strong. So that’s super exciting. We’ll make sure all of those links to that are in the podcast notes so people can check that. Thank you again.
Jon: Thank you.
-----
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 196.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Welcome back, you guys. We have had a break. We are back. I’m actually recording this before I was back, so I don’t even really know how I feel once this episode will be out, but nonetheless, I have been holding off and wanting to do this episode as the welcome back episode for the new season of Your Anxiety Toolkit.
 Today we have with us, my Assistant, my Executive Assistant, one of the most important people behind the scenes at CBT School and in my private practice. She is my intake coordinator. She is the doer of all things. She was originally hired as my Chief Copywriter. She does a lot of work behind the scenes for me. Her name is Elle Warren. Her and I have been working together for some time now. It has been such a pleasure to get to know her.
Today we have with us, my Assistant, my Executive Assistant, one of the most important people behind the scenes at CBT School and in my private practice. She is my intake coordinator. She is the doer of all things. She was originally hired as my Chief Copywriter. She does a lot of work behind the scenes for me. Her name is Elle Warren. Her and I have been working together for some time now. It has been such a pleasure to get to know her.
She today is going to share with you, just so you know, who it is behind the scenes if you’re ever in contact with us or you’re reading out Instagram posts or a newsletter or emails. She’s doing a lot of this stuff for me and we’re working together very closely. I wanted you to feel like you knew her, just like you know me. She also comes with a beautiful recovery story where she shares her experience with mental health and OCD and health anxiety, and grief, and post-traumatic stress disorder and experiencing, and really coming to find a place of peace with her sexual orientation. It is a beautiful, beautiful episode. I’m so, so excited to share it with you.
Again, I want you to feel like you know us. I want you to feel like you trust us and you know who’s behind the scenes, and that’s why this was so important to me. So, I hope you do enjoy the show. Elle really does share her story so vulnerably. If you do notice some background noises, Elle was in a really rural location, a lot of background noise. So, bear with us there. We were doing the best we can. I wanted to make sure we had this episode recorded before we left, so please bear with me. The content is still fabulous. I hope that isn’t too difficult on your listening.
In addition, welcome back. So thrilled to be back. I’ve been trying to do episodes through the school year and then take some time off for the summer. This season, we have some big plans, some amazing guests. I am really dialed in with specifically what I want to address this season. So, get excited about that.
I hope you’re well. I hope you’re being kind to yourself and you had a lovely summer and you had some time to rest and recover. I will share here very soon about our trip and what happened and what I learnt and what I experienced. I always like to refer to a couple of reflections later on, but first, I hope you enjoy this episode with Elle.
-----
Kimberley: All right. Welcome, everybody. This is a really wonderful start to another season of the podcast because I have here with me one of my core team members, Elle Warren. Thanks so much for coming on, Elle.
Elle: I’m so excited to be here. Thank you for having me.
Kimberley: All right. Let me share. I know everyone’s listened to the intro, but let’s just talk about how important you are as a part of helping me. I’m so grateful for all the work that you do to help me, so thank you.
Elle: Yes. I love it.
Kimberley: Yeah. The reason that you’re so special is because you’re so special. But in addition to being so special, you’re so wonderful as a part of this team because you get it. You get what we’re talking about, and that’s why I’m so grateful to have you on our team. I’d love to spend some time you sharing that story if you’re comfortable and telling us a little bit about your background. Do you want to give us an intro to your story?
Elle: Sure. Yeah. It is a long and winding journey, but I will try my best. I have had OCD for as long as I can remember, but I did not know that it was OCD until about two years ago. I was only actually diagnosed in February of 2020, so right before the pandemic, but I had been learning a lot on my own before that and came to that conclusion. Big themes for me growing up were sexual orientation, health anxiety, safety things. I remember I would always ask my mom for reassurance all the time. And then my mom passed away a little over three years ago now when I was 20, and that was the catalyst for my mental health feeling more unmanageable. I started having panic attacks. I was later much more recently diagnosed with PTSD from her illness and death and all of that as well. At the time, I just thought that my brain was broken, that I was broken. I can see now that it was just the intersections of OCD and PTSD and grief that is a pretty nodded up ball of things. So, that’s an overview.
Kimberley: When did you notice these symptoms first start? Was it in childhood, you said?
Elle: Yeah. I can definitely look back and see it in childhood. I remember one time when I was little, I don’t know, I was probably five or six, and there was a storm going on outside and I was so convinced that a tree was going to fall on our house. I remember I just kept asking my mom, “The tree was going to fall on our house.” That’s one example.
Kimberley: Did your mom suspect anything? I mean, was that something that was in your family, or was that just like Elle being Elle?
Elle: I think no one really talked about mental health in my family. I know now that there is a history of mental illness, at least on one side, maybe on both, but it wasn’t talked about at the time.
Kimberley: Isn’t it crazy when you find out, after the fact that you have this whole long line of genetics? It’s like, “Why didn’t I get told this information?”
Elle: Yeah, exactly. Right. It’s like, okay, there were definitely some signs that could have been. I mean, I don’t blame my parents. They were only doing what they knew and what they were taught, but it would have been nice if those things were acknowledged and then noticed earlier on and if treatment was offered earlier on.
Kimberley: Right. Sometimes it’s that our parents didn’t even know they had stuff. Often not even a parenting blunder. It’s like they had no idea the words to use to describe things either, right?
Elle: Right. Exactly.
Kimberley: Yeah. Do you want to share that about your themes? For those who are listening, we will share at the end that you’ve written some amazing blogs for us and we will make sure we have those in the show notes, but do you want to share about the specific themes that you’ve struggled with?
Elle: Yeah. I think the most significant one, like I said, was the sexual orientation one. That was definitely the one that I can remember taking up the most time and causing me the most distress. One day when I was probably 12 or 13, I was in middle school and I remember I was sitting on the sidelines at cheerleading practice and I had this memory come back to me of this girl in my neighborhood that when we were little, we used to kiss sometimes, which is a very innocent thing. We were four years old. But I agonized over that and wanted to know what it meant and be certain of what it meant. I grew up Catholic and I grew up in a relatively more conservative area, so to me, the idea that I could be anything besides straight was just unthinkable. I think I said this in my blog post about it, but almost equivalent to remembering I had killed someone or something super dramatic like that.
Kimberley: And that was because of what you’d been taught?
Elle: Yes. Really from the ages of 13 to 20, 21, that was a really big thing. It would come in and out, like I’d let it go for a little while, and then it would come back in full force. I would be imagining scenarios in my head all the time and trying to predict how I would feel in them. I would look at people when I was out and ask myself if I was attracted to them and all of that. Now, I identify as bisexual. I think that adds to it as well because bisexuality is often invalidated and there’s the pressure to pick a side and all of that. I didn’t really know. I didn’t know much about my bisexuality. I didn’t know anyone that was openly bisexual. I didn’t see people on TV that were bisexual. I think it was not only hard for me to accept that I could not be straight, but it also didn’t really feel like a possibility that I could be open to more than one gender.
Kimberley: What was that transition like? It sounds like from what you’ve told us, there’s this absolute struggle with this idea at the start and it being a lot of uncertainty. I think you’re mentioning you have a lot of rumination around that. How did you get to the place where you are now?
Elle: After my mom died, about a year after, I ended up moving from Michigan to Denver. Denver is what I would call a fairly liberal city. I knew a lot of people that were open with their sexuality and I wasn’t around the people that have known me my whole life, because it’s a lot harder to go against the expectations of people who have known your whole life. It’s different when you can create the self that you feel like you are when you can start with that.
I think I felt like I had the freedom to explore who I really was. I knew I had people that I could identify with. Also, I think the experience of losing my mother, who was the absolute, closest person in my life, I think it just made me less afraid, in general, because, it sounds cliché, but it was like, you’re hit with the fact that time is limited, and you don’t want to waste it. You don’t want to waste it by being unhappy or hiding parts of yourself. I think in general, it just made me a lot less afraid and less timid because I realized that if there’s so much out of my control, I’m definitely not going to waste time not being who I am.
Kimberley: You move from a place of being uncertain to just fully accepting radically who you were and just waited to land wherever you landed. Is that how the shift was?
Elle: Yeah, pretty much. I don’t know. I remember I was laying in bed one day trying to go to sleep and it just went off like a light bulb in my head. I was like, “Oh, I’m--” other times, pansexual has felt more, right? Truthfully, I don’t get too caught up in a specific label, but at the time I was like, “Yeah, I’m not straight.” It just went off like a light bulb. I think maybe the groundwork for that was laid by the radical acceptance that I had cultivated for my mental health, because like I said, after losing my mom, my brain and my nervous system really went into overdrive and my mental health was really, really, really a struggle. But at that point, I had cultivated a lot of acceptance and self-love for that. And so, I think maybe that foundation was laid there and then paved the way for me to also accept my sexuality.
I think I just realized that it actually doesn’t matter that much. These days, I embrace the uncertainty. Like I said, I don’t care that much about the label. If bisexual feels right now, cool. If lesbian feels right one day, cool. I more so just have the attitude of like, I’m going to date who I want to date and listen to my heart. The certainty doesn’t actually matter.
Kimberley: Yeah. It’s such a cool concept too. I think a lot of the interviews I’ve heard around sexual orientation is like, “Oh, I had all this uncertainty and I did the treatment and none of my fears came true or whatever.” You know what I mean?
Elle: Yeah.
Kimberley: I love that you’re really walking the walk because you had fear and uncertainty and you just continued to be uncertain. It’s not like you have some resolution at the enemy. There was. But I love that you’re just in a place of just being at it. It is what it is. I feel like that’s a story that’s missing when it comes to sexual orientation OCD.
Elle: Right. I think that’s a really good point because it’s true. The uncertainty didn’t go away. My attitude on the uncertainty just changed. I think you’re getting over the hump of shame that comes along with non-heterosexuality is a big part of that too, because I’ve seen on social media, I feel like a lot of people, it really scares them that someone else who had sexual orientation OCD actually turned out to be not straight. I think that that’s scary for a lot of people. That’s a whole other thing. That’s not just OCD, that’s the shame that many of us have grown up associating with non-heterosexuality.
Kimberley: Right. That internalized stigma that is placed on us.
Elle: Right.
Kimberley: I really love when you wrote that article and we will share it again, and you share a lot of this story. I really do love it because I really worry sometimes when I see Instagram posts and things of like, “Everything I’ve ever worried about never came true.” You know what I mean? I see that’s true for a lot of people, but it is a form of reassurance almost of like, “Don’t worry, your fear is just a thought.” I think this is an opportunity to fully embrace these concepts. The thing I love about what you’re talking about the most, and I don’t hear enough people talking about it, is it’s coming from a place of just genuine love. Not from a place of like, “Well, my therapist told I have to radically accept it.” You know what I mean?
Elle: Yeah. Right.
Kimberley: Yeah. Thank you for sharing that. I’ve just loved that story so much, even though I hate that you have gone through a difficult time. You talked about your moms and the grief around that, you talked about how her loss helped you move into radical acceptance, but how else did that impact you and your recovery or your struggles?
Elle: In so many ways. The person that I was before and the person that I am now are two very, very different people. I think the biggest thing is like, my mom and I were very close. I’m the youngest of four kids and I’m the youngest by a lot. So, I definitely got my parents, especially my mom, all to myself a lot. I was very emotionally dependent on her. She was a huge source of love and the most loving mom that I could have asked for. That said, I hadn’t really learned how to mother myself, how to be my own source of love and affirmation, and all of that. That’s terrifying to just be dropped into.
I think the ideal situation, if we all got to have ideal situations, would be that we gradually get to that point. We grow into adulthood while we still have that support, which is the same, my dad is supportive but in a very different way. I felt like there was no one there to hold me up or to witness me. I just felt very alone. She was, I think, the person that I was the most vulnerable with. So, not having that just was really scary. I didn’t know how to cultivate that in myself for a long time. I do now, which is a really good thing.
Kimberley: How did you learn that? I feel like I don’t know how to do that really, really perfectly. You know what I’m saying? I think there should be a course in middle school that teaches you how to do that.
Elle: Yeah. There should be. I think part of it is like, what I learned from her in terms of how she cared for me, I think that I tried to replicate that for myself. There’s a lot of trial and error and it was a lot of not wanting to do it, but I’m making myself do it just in terms of making myself meals, getting out, and going for a walk. Very basic things. Because when you’re in the thick of something like that, the basic things are still hard things. I think it came from this almost outside source of love that I have for myself and the life that I know that I want for myself. It was like, I knew that I deserved that and I knew that I could get there someday again. This is a cliché metaphor, but I felt like I just needed to climb this mountain. I felt like I just needed to keep taking steps. And then maybe eventually, I would be able to see out over the top.
I do have other familial support as well. I have siblings and my father. In terms of some other ways, it’s affected me. It definitely did not help my health anxiety because throughout the time that she was sick, there just were a lot of fluke things that happened, a lot of things where doctors would be like, “Huh, we’ve never seen that before,” things like that. So, that has been an increased challenge.
Kimberley: Are you still working through that? I mean, that has to be really scary because that’s what the voice of OCD says, right? Like, “This one symptom is one of the symptoms that’s going to kill you,” kind of thing. Given that that was your experience, how are you managing that?
Elle: It’s definitely gotten better over the years. Something that I still struggle with, it’s-- I dunno. I’m a lot better at recognizing when I’m in an OCD spiral. I can usually, most of the time, be an observer of it and notice what’s happening. I also did choose to go on medication just earlier this year. For me, that has been really helpful.
Kimberley: And that helps with the health anxiety or for the grief or for a combo of all?
Elle: It’s helped in a lot of different ways. Honestly, it’s helped with the PTSD symptoms a lot and it’s helped with OCD symptoms. It’s helped with depression symptoms. I mean, it can be hard to pick out which is which because they all feed off of each other. I feel like even if it’s really just helping with one of those things, it helps all the other areas too. But just in general, it’s been a game-changer.
Kimberley: What degree did you have to practice exposure and response prevention for all of these symptoms? Was that a part of your work? How did you navigate all of that? Did you do it on your own? Did you have a therapist?
Elle: I have only practiced ERP on my own. I have a therapist that I was working with for quite a while. I think I was seeing her regularly for probably two years. I found out, this was only maybe six months ago, just through us talking, I learned that she didn’t understand OCD really at all. So, I don’t see her anymore. I just try to do ERP on my own every day, and that has worked for me so far, honestly. I would like to work with an ERP-trained therapist at some point, but right now, that still has made a huge difference.
Kimberley: Right. How was it to do it on your own? I mean, a lot of people, this is a common question I get – “Do I need to have an ERP therapist?” Of course, with CBT School, we have the course. We have ERP School. “Is that enough? Or could I do a workbook or could I just go off of what I’ve seen people do on social media?” How did you bring yourself to do that? Is it just by your own education? How did you learn?
Elle: I feel like I started doing it really before I even knew what it was called, before I even knew that it was like a thing because again, I just kept going back to the vision that I had of myself and who I wanted to be, who I knew I could be, my love for myself. But I think that that can sound really romanticized like, “Oh yeah, I just did it on my own, and I’m pulling myself up by my bootstraps.” But it was hard.
In retrospect, I probably should’ve asked for more help than I did. I mean, I don’t fault myself for any of this because you can’t know what you don’t know, right? But I wish I would have been more honest with the people in my life about how poorly I was really feeling. I’m proud of all of those exposures that I did every day. Sometimes it feels and felt literally like you’re walking into the jaws of a shark and you don’t know whether or not you’re going to come out. It really does feel like that. That’s not easy. I think having someone to support you through that and walk you through that is probably really helpful.
Kimberley: Right. It sounds to me like you use naturally a lot of, and I could be wrong here, tell me if I’m wrong, but a lot of what we would call acceptance and commitment therapy tools, like your values really left you, led you down the road you wanted to be at like, “What do I want with my life?” Sometimes that voice and that question, remember, we talked about asking good questions. That’s a really good question like, “What do I want for my life?” I think that can sometimes lead us in that direction. Would you agree with that?
Elle: Yeah, I would. I think that that is what was carrying me through a lot of the time.
Kimberley: Right. I have one more question if you’re willing to share. What was it like for you to have PTSD? A lot of people I know have either been misdiagnosed with PTSD and then find out they have OCD or they find out they have both. What did that look like for you?
Elle: For me, it was a lot of not being able to focus, not being able to be present. I felt really depersonalized and/or derealized much of the time. The panic attacks again, like I said, and the memories always felt very close. They didn’t feel like things that happened a while ago. They felt like things that just happened. Honestly, that’s been a big difference that I’ve noticed with the medication is that I can say they feel they were things that happened a long time ago. It’s still painful, yes, blah, blah, blah. But it happened a long time ago. The way that I would describe it at the time, I remember thinking about this metaphor, it felt like my brain was just this mass of cross wires that were sparking, and again, it felt broken.
Kimberley: Yeah. That’s a really interesting metaphor. I think a lot of people would really resonate with that. Memories, cross wire, everything’s misconnected, and so forth.
Elle: Right. Because it changes the chemistry of your brain.
Kimberley: Right. Yeah. Thank you for sharing that. It’s something we don’t talk about a lot. It's something that I’m actually in the process of being trained on more extensively because I think a lot of people do have PTSD and it has been misdiagnosed or underdiagnosed. I’m so grateful that you’re sharing about that. Thank you. I know it’s not easy to share that stuff.
Elle: No. I’m honestly really grateful to be able to because I think younger me would have appreciated hearing something like this a lot.
Kimberley: Well, before we finish up, I have a couple of questions, not related to your mental health, but just more related to you and I because I love what you’re sharing here. I’m so grateful you shared this information because I think there’s a story here that I think a lot of people may resonate with or be appreciative of to see that you’re on the side where you’re at right now. It’s very cool. What is it like to work for a CBT School? Go ahead. I didn’t tell you I was going to ask you this question. You can be as honest as you want. What is it like for you to work in the work that we do? And again, you don’t have to make it sound good.
Elle: I’ll tell the truth. I appreciate being able to share information that, again, I would have needed or has been helpful for me along this journey. Also, they’re good reminders for me. If I’m writing something about self-care or whatever, then I’m like, “Okay, it’s a good reminder. Okay, I need to practice what I preach.” They’re good check-ins. Also, doing it on social media platforms is just a really powerful reminder that, “Oh yeah, it wasn’t just me. This isn’t just me. Lots of people feel this way, and they also have worried that it was just them.” That’s really connective. Obviously, you relate to this – I need to be fulfilled by my work and I need to feel like it’s purposeful and I need to feel like it’s connective, and it is those things.
Kimberley: Am I just the biggest pain in the butt boss you’ve ever had? You can be totally honest. I am totally a pain in the butt boss. I know I am.
Elle: No. I do tell people how much I like working for you. You have been definitely, I would say, the most understanding and flexible boss that I’ve had.
Kimberley: I think that’s because I was going to say, nearly every staff meeting, we made it almost this time. I think every single time I go, “You’re going to have to bear with me. I’m all over the place today,” I have to apologize for how messed up everything is. I’m like, “You’re going to have to forgive me. I have no idea what I’m doing.”
Elle: Right. It’s like we’ve said in posts before, like being imperfect, it gives other people permission to be imperfect.
Kimberley: Right. I agree. Thank you. When I asked this, I was like, I wouldn’t doubt if she was like, “Oh boy, I feel uncomfortable, I don’t want to tell you the truth.” For those who don’t know, Elle and I meet, and we go through probably 40 things we have to get through. We have this whole list of social media or newsletters and podcasts and SEO and websites and all these things. I think every time I started going, “I really have no idea--” I will add, which I think is hilarious, is that Elle went on a vacation recently and asked me to do some of her jobs. I actually had no idea how to do that. I literally had no idea how to do the jobs that you do for me. Thank you so much for being my friend and helping me in those moments.
Elle: Yes, absolutely.
Kimberley: Right. I’m like, “I have no idea how to call my own clients,” or “I have no idea how to write my own email here, help me.” I’m so grateful for the work that you do. I think that you have a voice. Again, you actually came on to CBT School as the copywriter, as our Chief Copywriter, and your voice is so exactly the voice we need. Your compassion and your experience and your kindness – it’s wonderful.
Elle: That’s awesome. I’m so grateful that we have found each other.
Kimberley: Yeah, me too. I’m so, so grateful. Before we finish up, tell us where people can find out about you or get your information. Besides the work we do here, where can they get your personal stuff?
Elle: Yes. You can find me @griefgurlwithocd on Instagram. I spelled girl G-U-R-L, and everything else is spelled normal. I’m not super active on it, but I do love getting messages from people. Feel free to reach out there.
Kimberley: Thank you. All right. Everyone, I’ll link the blog that you wrote about sexual orientation OCD. They can read that too. Thank you so much for coming on.
Elle: All right. Thank you.
-----
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 195.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Kimberley: Hello there. I have with me a very special friend who is going to talk about something so important. So, so important. I am so excited to have with us Shala Nicely. Oh my goodness, thank you for coming back onto the show.
Shala: Thank you so much for having me. I love being here.
Kimberley: Oh my goodness. Okay. So, probably the reason that I have been so adamant about getting you onto this episode is this topic that we are going to talk about is probably one of the topics that comes up the most with my patients and clients that nobody is talking about.
Shala: Yes.
Kimberley: Nobody. And I am seeing it more and more and more and more and more, which is why I wanted to have you on. So, thank you.
Shala: Yeah.
Kimberley: Thank you. Okay. So, you wrote a blog about depression as a compulsion. Can you tell us what does that mean?
Shala: Yes. I’ll start off by saying that this is one of the many subtleties of OCD. Sometimes OCD takes a long time to figure out. I spent years becoming a therapist. I spent years thinking about my own experience and when I was writing my memoir Is Fred in the Refrigerator?. It wasn’t until after Fred was published, that I figured out this particular compulsion that I had been doing. By identifying it, it’s been able to help me make a huge difference in my recovery, and that’s why I wanted to share it and write the blog.
Kimberley: Right. It’s so important. I mean, I can’t tell you, I’ve been practicing for many, many years and I only came across this in the last year or two. But the more I get to know it and the more I understand it, I’m just like, I feel like I see it in almost all the cases in some way. So, go ahead. Tell us what it is. Tell us what it looks like.
Shala: So, I’ll give you an example that I used in Fred, which is, when I was in my twenties, I was convinced I’d given myself HIV aids because I had gotten cut with a broken beer bottle at a party and I had spent all this time in my head arguing with OCD about whether or not that you can transmit HIV aids through that. It went on for months and months and months. While I was doing all this ritualizing in my head, trying to figure this out and prove to myself I didn’t have this disease, which this was years and years and years ago, the treatments for HIV aids are much better now, they weren’t. This was 25 years ago. I know people with OCD are still frightened of it. I was really frightened of it back then because there weren’t very many treatments for it.
And so I would spend all day long thinking about how I had given myself a fatal disease and how I was going to die. And then I started acting as though I had a fatal disease that there weren’t good treatments for and I was going to get it and die. So I would go into situations and put on a happy face and smile, but in my head, I was thinking, “Oh, this is the last time I’m going to be doing this. Oh, this is so sad. Just wait until people find out what is really going on with me.” So I would focus in those situations on how awful this was and how depressed I was and how this was going to be the last time I was going to do it.
So, I was actually acting as though what OCD was telling me, which is that I’d given myself fatal disease, was true. And the depression that came from that became the compulsion because I took that emotion and I acted on that emotion. So I started acting depressed, making depressed choices, living in a depressed lifestyle, having a depressed attitude as I went out into the world because I had given in completely to what OCD was saying.
When I realized that, again, this was after I’d written the story, after it had been published, and I started seeing this in my clients. I started recognizing I still did some of this. I’m like, “Wait a minute, it’s the depression itself, which was really propping all this up.” It’s really a very subtle form of compulsion that if you don’t recognize it can sabotage your ERP work.
Kimberley: Yeah. I would admit as a young intern of treating OCD, I think if I saw this, I would have stopped ERP and focused on depression and really worked on that, which is not a bad solution, but without really recognizing it under the lens of OCD, right? So, I would have seen it as separate. I love it.
Let me explain how I’ve seen it a lot. Once I’ve shown them your article, patients and clients have said, “I recognize in the moment that I’m having uncertainty. I try doing a compulsion to make the uncertainty go away and that doesn’t work. So, going into depression is our easy way to just exit out of uncertainty. It’s the worst-case scenario. That’s where I’m going to hang out.” That has been so helpful for people to be able to recognize that. It’s a response to not wanting to be uncertain.
Shala: And I think it’s important to differentiate between depression that comes secondary to having a diagnosis of OCD from this, because a majority of people with OCD will end up with some form of depression at some point, because it’s just so debilitating. It’s the 10th most debilitating condition in the world. So people will end up depressed just because of how exhausting it is to manage this monster in your head all day long.
But that’s very different than being depressed because you’ve decided to believe that the OCD is true because you cannot figure it out otherwise. And OCD just wants certainty. It doesn’t care what kind of certainty it gets. If it can’t get certainty, for instance, that I don’t have HIV aids, it’s just going to go the other way and say, “Well, I’m going to get certainty that she does have it,” and then go from there and then becoming depressed as a result of that obsession. So, I think that’s really important for people to understand. You can have both going on at the same time too, which makes this even more tricky.
Kimberley: Yeah. Even more tricky, but even great to know that we can differentiate the two now, because we’ll talk later about how to manage that. Now, this is where I want to look at insight because, in your blog, you talk about insight. I think that’s an important piece of this, right? Because when you first have the onset of OCD, you might recognize that this is like ego, what we would call egodystonic, like this stuff. “I know it’s not true, but I keep fearing it’s true.” Can you share how insight impacts this specific situation?
Shala: Yes. In fact, it was Jon Hershfield who introduced the two of us years ago, who helped me put this insight about insight together, because I was talking with him about this depression is a compulsion. What he pointed out is that typically, when an OCD obsession starts, you’re doing compulsions to try to prove that it’s false. If you can’t get that to work, which of course you can’t because there’s no way to prove all this stuff that I see he’s worried about, then sometimes you can start going the opposite way and trying to prove that it’s true. Really that’s the difference between insight.
When you’re trying to prove that it’s false, then you know that what OCD is saying in some part of you is nonsense. “I don’t have HIV aids, come on.” Not like in a reassuring way, just there’s a part of you that still recognizes, “Yeah, this is super scary, but this is OCD reacting to an intrusive thought. This isn’t actually a real problem.” So, you’ve got that insight there. You’re still stuck, but you got insight.
When you start trying to prove it’s right, that’s when you’ve lost insight. When you really give in to everything that OCD is saying, really hook, line, and sinker, and you don’t have any insight anymore. That’s really when this depression as a compulsion becomes a big problem. The longer that a particular obsession is maintained by doing compulsions, the more likely you are to lose insight, the longer it’s been going on.
Kimberley: And this is where it’s hard, isn’t it? Because we know the whole story of when you stare at something for too long, it starts to look weird and distorted. I think that’s very much true here. I think it’s true of depression in general and in this subtle compulsion. When we look at things as negative, we notice more and more things that are negative. Is that what you feel to be true here? Or is it just the same story that you hear over and over? Share with me how that might sound in your head.
Shala: I think it starts to sound like a soundtrack for my life because most of my rituals became internal. And the way I see mental rituals, it’s physical rituals taken inside. So you can’t do things physically because you don’t want people to see or whatever. So you start pulling it inside. The more that I would do that, the more I would argue with OCD, of course, the more I’m strengthening in it. So the more I hear it and the more I argue, it just expands to fill every waking moment. It really becomes a soundtrack playing 24 hours a day because I was doing those mental rituals. And then the longer that that went on, the more likely I was to start becoming depressed because I was losing insight, which then also further reinforces this cycle.
Kimberley: So interesting and so helpful. One thing that you talk about is emotions as a ritual. Can you share how this may play out with other emotions such as – you’ve written guilt and shame, regret and grief?
Shala: Yes. So what I’m going to do to describe this is I’m going to take you through the OCD cycle in some anatomical details, so to speak, so we can piece together how this is all happening. So you have an intrusive thought. That is not OCD because everybody has intrusive thoughts. The OCD is the next stage where OCD reacts to the intrusive thought – “Why did I have this? What does this mean? Am I going to do it? Am I going to make it come true because I have the thought?” That reaction, that’s the OCD. Of course, that makes you feel anxious. And then if you haven’t had treatment, you typically do some form of compulsion, something to try to get certainty about what the OCD is bothering you about, because this is all based on an intolerance of uncertainty. And OCD just picks content that you care about and puts uncertainty about it in your mind and then gets you stuck in that cycle.
When you do a compulsion, it tells your brain that this is a dangerous thought, “This intrusive thought I had is dangerous,” and you need to keep doing something about it. These steps just repeat on an endless loop. And then what happens is that when it repeats on the loop long enough, the acceptance of the scary thoughts that OCD is presenting causes you to experience the emotions that you would feel if those stories were true. Those emotions tend to be things like depression, as we’ve talked about, guilt, regret, shame, grief, and others.
And then in classic cognitive behavioral therapy perspective where our emotions and our thoughts and our actions all come together in this triangle, the emotions then dictate how we act, so we begin to act depressed or guilty or regretful or shamed or grief-stricken. Those emotions can then become compulsions because they’re driven specifically by believing the content of the OCD, by acting like what OCD is saying is true. That’s the definition of doing compulsions. So that’s how emotions can become part of the compulsion cycle because you start acting as though they’re true.
Kimberley: Right. This is so true and this is where I see it play out a lot, is when people have an intrusive thought that they’ve done something wrong, and then they feel... Because they start to believe it, they go into regret and then they go into confessing, right? Then they’ll go into like, “Well, I have to confess it because I’ve done something wrong,” instead of that they had a thought that they did something wrong. Or that they feel such deep guilt that they’re saying things like, “I’m a terrible person. I’m terrible. And I’m so guilty. What kind of human am I?” because of a thought like you’ve just described, how then that plays out and keeps playing out over and over again.
Let’s play out because we haven’t really talked about this, but what would the action be as a result to regret? It would be reassurance seeking or confessing. What else would you say?
Shala: Maybe going back in your mind and trying to undo it and, “Gosh, what would it be like if it had only gone like this?” Almost like a wishing compulsion that I think [14:22 inaudible] talks about in his book. All sorts of things like that.
Kimberley: What about guilt? Similar, but what about guilt?
Shala: I think with guilt, it’s a lot of self-punishment as a ritual. “I’m bad. I did something bad.” With guilt and shame, guilt is, “I did something bad,” shame is, “I am bad.” I think in this case, those can get conflated together and people just start punishing themselves. “Well, I don’t deserve this because I did this bad thing,” or “I am this bad person.” They start being very uncompassionate with themselves and treating themselves like they’re this horrible human being.
Kimberley: Right. And that’s a big part of how I see it play out is that the self-punishment is pleasure withholding, like you don’t deserve the nice-- it could be as subtle as you can’t have the nice brand of crushed tomatoes. You have to have the crappy brand because you don’t deserve good things or you don’t deserve the nice sheets or so forth. And that will make you feel-- when there’s no pleasure in your life, you get depressed, right? I think that’s a very subtle way that OCD plays out. I’ve heard lots of people will say, or the flip side is they’ll say something like, “Oh, because I have harm thoughts about my child, I have to buy them the best diapers,” which is treating yourself as if you’ve done something wrong.
Shala: Yes. You’re making up.
Kimberley: You’re making up for something that you had a thought about, right?
Shala: Yeah.
Kimberley: Right. It’s so subtle. What about grief? Can you kind of give an example of that?
Shala: I think with grief, it’s pre-planning things. So, for instance, I’m not kidding you, I’ve pre-planned my funeral in my head – “Well, this is what it’s going to be like. It’s going to be so sad and I wonder if this will happen and that will happen,” as though it’s an event two weeks from now on my calendar, Shala’s funeral. So I think it’s almost like you act like the loss has occurred already and you begin to start going through the grieving process.
People with OCD tend to be really empathic people, so it’s really easy to go there. It’s easy to put yourself in that, “Oh, so-and-so has died. This horrible thing has happened. Let me go ahead and get into that grief state,” because we’re just good at being able to put ourselves in other people’s shoes to imagine what something would feel like, and to feel it as though it were happening.
Kimberley: It’s so good. All right. So--
Shala: Can I say one more thing?
Kimberley: Of course.
Shala: Sometimes I think of these as fake emotion. They’re not, right? But they’re OCD-induced emotions.
Kimberley: They’re manufactured.
Shala: They’re manufactured. They don’t actually fit the truth of the situation. I’m not saying they’re fake like, gosh, the shame you’re feeling or the guilt you’re feeling isn’t real. Certainly it’s a real emotion, but I think it is induced completely by the OCD, as opposed to being induced by a situation that has happened in life.
Kimberley: I agree. And that’s where that insight is really important, right? Is to be able to catch that. I fully agree with you. I’m so glad that you recognize that because people will say it feels real, right? It feels real. And then I’ll always follow up with like, “But it’s not a fact.” But still, it’s important to have that conversation.
Now, I want to just jump in here. Before we talk about how to break this cycle, how might this play out with just Right OCD?
Shala: I can give you an example from yesterday about this.
Kimberley: All right.
Shala: I decided I was going to get these floating shelves and hang them on the wall. It requires using a drill and all sorts of things, which I can do, but I’m not very good at it. I also, I guess, was sort of distracted and I’d had problems with one of them and with the drill, as I went downstairs to do the other one. I put the shelf a couple of inches too high because I used the wrong mark on the wall, probably because I was exhausted from having drilled drywall over the place and making a huge mess upstairs. Once I got the shelf installed, I’m like, “Oh, what’s that little mark on the wall? Oh, that was where it was supposed to be, a couple of inches higher.” I am not redoing it because it made a huge mess in the wall and it’s going to have to stay there. My OCD put this little feeling in my stomach. “That’s just too high. It’s wrong. It’s horrible.” I could feel it. Like, I feel it right in my solar plexus, this little tightening, like, “Oh, we can’t stand this.”
What I decided to do, because I am not moving that, I just say, “OCD, this is great. I am so glad that shelf is at that level. I’m glad, number one, because it’s upsetting you. But number two, it actually probably is a good level because I have a big dog who likes to bounce around on the couch. This is above the couch. If it’s actually too low, he’s probably going to knock his head on it and knock it over. We’re just going to live with it. There are some good things about it being at this level, just like there’s some good things about it being at another level. I’m just going to smile and be happy every time I see that shelf.” So, when I see the shelf now, I really try to have good, positive, happy emotions about the shelf being at that level and tell myself, “We’re not changing it. OCD, if you don’t like it, fabulous.”
Kimberley: Right. But originally, was it that you would slip into a depression as a compulsion?
Shala: Yes. So, what happens with Just Right OCD that can have this same thing go on is we look at the shelf every day and go, “Oh, it’s ruined the house. The house is not perfect because the shelf is in the wrong place. If we could just move the shelf down.” And then you envision moving it down, but then you think, “Oh my gosh, it’s going to open up more holes in the drywall, and then I’ll have to fix that. I can’t do that. If I’d only been paying more attention.” Everybody can’t see this because they’re not watching the video of this, but if you can see my posture, it’s like--
Kimberley: It is. You’re getting low.
Shala: Like, “I screwed up and now it’s bad and I’m depressed.” And then every time you look at it, you have those regretful thoughts and you think about, “Gosh, how I’d like to change that.” And that causes more regret. And then that fuels the whole emotions as a compulsion cycle.
Kimberley: Which is interesting. I think this is true for any subtype. And you may correct me on this. The thought that I hear the most is, “This is going to bother me forever.” That’s where I feel like the depression as the compulsion set seen as like, “You’ll never have happiness again. This is going to be the worst.” And then you go actually, like you sunk down into that. You sunk in and you stayed into that kind of mindset. Is that an example you would give as well?
Shala: Yeah. I think with any Just Right OCD, it’s this feeling that life is somehow ruined because this thing is wrong. Ruined means forever. It’s all blurry, black and white like you were saying. So it feels not only unfixable, but unbearable, and then giving into that and then acting as though this unbearable thing has happened, then becomes the emotions as a compulsion. I think this is probably pretty common within the whole Just Right OCD thing, is having so much regret that it’s not right, then act as though that regret were true.
Kimberley: Right. Well, okay. So, that’s the perfect segue, is how do we break this cycle? How do we intervene? Where do we intervene in the cycle?
Shala: The way that we intervene in this cycle, through exposure and response prevention obviously, is doing the acting as though the content that OCD is threatening you about or bothering you about is irrelevant. Let me start out by first saying how people tend to make mistakes doing this because I think this is important.
So, as we know with exposure and response prevention, we’re exposing ourselves to the uncertainty of the obsession while not doing compulsions. If you have emotions as a compulsion, depression as a compulsion, you can do an exposure. Think you’re not doing compulsions because you’re using scripting to get out of your head. You’re not asking for reassurance. You’re not doing your physical compulsions. But you’re still bummed out, regretful, ashamed. So you’re doing it while in your head, really spending a lot of time in that emotion. So you’re really doing exposure without response prevention. You’re doing some response prevention, but you’re not doing enough response prevention. So the exposures don’t work very well.
People can get stuck in this cycle where they’re doing ERP over and over and over again and they think that they’re getting rid of all these components and they’re not getting better. It’s probably because something like this is going on in the background where they’re still, at some level, believing this and acting as though it were true. So, that’s where people make mistakes.
What we really need to do here is find that little bit of joy because it’s there. It’s probably been so covered up by the OCD, the depression, whatever other negative emotions you’re experiencing, that you don’t think it’s there, but it is there. You can take yourself back to when you were really happy about whatever it is, like, say that you think you’re going to harm your children. And you can remember times that you were with your kids where this wasn’t bothering you. So, you take yourself back to that and you think, “How was I acting? What was I doing? How was I feeling?” You find that and you go do those activities and you focus on that joy. So, when the OCD says, “Oh no, we can’t, we can’t. You’re irresponsible. We were going to kill them. We’re going to harm them. We have to focus on how bad we are,” you’re like, “Nope, I’m going to focus on how much fun my kid is having in the pool. Isn’t this great? It’s a sunny day. Really enjoying it. It feels so nice to be out here. Look how happy my kids are.” You just find all of the joy you can and you focus on the joy.
What we’re trying to do here is act as though the content is irrelevant. So, if you’re acting like it’s relevant, you’re standing in the pool with your kids going, “Oh my gosh, this is terrible. I’m going to kill them. They’re happy now. But just wait until I kill them and their mother finds out or whatever, that it was me.” Or you can be in the pool like, “This is great. I love spending time with my kids. This is awesome. Look how much fun they’re having. They’re doing so well with their swimming. They’re having a great time. They could probably stay in here until they turn blue. This is great.” You’re acting like all that stuff in your head about the fact that you might harm them doesn’t matter. And that’s the essence of good exposure.
It really takes this finding joy because you want to do the opposite of what OCD is saying. OCD says you should act depressed, regretful, ashamed. So you say, “I’m going to do the opposite of that. I’m going to act happy, jubilant, carefree.” And that’s how we do these exposures. It’s not easy, but if you get good at it, it can be really revolutionary in terms of your recovery.
Kimberley: I love this. So, I’m thinking of one particular person right now, and it’s a follower actually. What would you say, because I love everything you’re saying. What would you say to the person who then may start to do that as a compulsion too?
Shala: Yes. I think that OCD can turn anything into compulsion.
Kimberley: It’s so skilled. There’s such skill. So
Shala: Yeah. I think that that is a potentiality for anything that we do with ERP. We are not doing this to make your anxiety go away. In fact, you’re going to be more anxious while you’re trying to find this joy because you don’t deserve to be joyful. It is not responsible to be joyful. It is tempting fate to be joyful. So you’re going to be--
Kimberley: Irresponsible is the word.
Shala: Yeah. You’re going to be having maybe 5% joy and 95% anxiety if you’re doing this right. If you make this compulsive, you’re doing it to reduce anxiety. I’m so glad you brought that up. That is what we’re looking for here, is this is going to make you more anxious. And the more that you do it and really find the joy and act like you’re having fun anyway, eventually, the anxiety will subside. Who knows when? It may take hours, days, weeks, months, whatever. But that is not the goal. The goal is to be in the situation while being anxious. And the more anxiety, the better, right? Because that means you’re giving your brain a good learning experience. That means that you’re doing things that help you tame OCD and reclaim your life.
Kimberley: Right. Thank you so much for sharing that because that’s such a crucial piece – to be able to integrate joy and anxiety in the very same moment. If you could do that, you’re winning, right? You’ve won, because OCD wants you to integrate anxiety and depression at the same time. So, I love that that is the way to give OCD birth ultimately, is to show that you can do that. I love it.
So, let’s talk about one more thing. I want to be respectful of your time. Someone has had OCD for a long time, obviously, because this has gotten so stuck. They’re having a lot of this depression as a compulsion. We’re asking them to find things that used to bring them joy or look back to a time where they could integrate anxiety and joy at the same time. What are your thoughts around “Fake it till you make it”? Is that an approach that you would consider? I know you’ve talked about other ways. Would you like to share your thoughts on it?
Shala: Yeah. I mean, there’s nothing inherently wrong with the “Fake it till you make it” stand, except for if you’re saying you’re faking it, you’re saying that there is no happiness there. And that’s almost giving in to the OCD once again. So, what I like is a different way of phrasing it, which comes from a woman named Heather Hansen who wrote a great book called The Elegant Warrior. We’ve both been on her podcast. What she says is, “Show it till you grow it.” I love that because that acknowledges that the positive emotions are there. The OCD is sitting on them and squishing them and you can’t feel them, but they are there. That also reinforces this notion that the OCD, this is a bunch of content it’s making up. It doesn’t feel like that, but these are things that it has imposed upon your life to make you worry about them. But you’ve got this great life that sort of smushed down underneath it. And you just need to find a little bit of what that great life used to be and find that and grow that.
It’s almost like if you think of a black canvas and then there’s a little pinprick of light, sunlight and it comes through as like a ray. And then the ray comes through and it starts to makes the black cloth start to have the hole, get bigger and the sunlight gets bigger. And then the sunlight comes through and eliminates everything. That’s what we’re talking about here. It’s just a pinprick. It’s a tiny bit, but it’s really there. If you say you fake it till you make it, you’re not giving yourself the empowerment you deserve, that it is in you. It is there. You just don’t feel it because of the OCD.
Kimberley: Right. It is. It’s like a muscle that you grow. I agree with that. I think that that is exactly perfect for it because, like anything, if you’re trying to get 100% joy, you won’t get any joy. But if you give yourself permission-- because we can get perfectionistic about this and be like, “Well, no, this used to bring me so much joy.” So I think you’re right. It’s just little baby steps and little baby pinpricks is the way.
Shala: I’m so glad you brought that up because like all of us with OCD can make things compulsive. We can also try to do our therapy perfectly and try to do these exercises and go out and be like, “But I wasn’t totally happy. I did have some intrusive thoughts. I did feel some depression.” Yes, of course. You’re going to. So, I think recognizing this is a process and what we’re trying to do is find the 1%, the 0.05%, the 3%, the 15%, whatever it is of joy and focus on that. Yeah, you’re going to have those depressed feelings. They’ve been there for a while. By the time you have depression or other emotions as a compulsion, it’s probably been there a while.
So, this process of ERP is also going to take a while and it’s challenging and it’s hard. So, you’re not going to go out and do this perfectly. You’re not going to go have some awesome experience with your kid. You’re going to be acting as though you’re having an awesome time. You’re going to be trying to focus on that in your head. But the vestiges of the OCD and those other emotions are going to be there. Let it be there. We’re not with this trying to shove those away necessarily and not feel them. What we’re trying to do is focus on the ones that actually match the ERP, which is, if I’m going to go focus on being with my kids and having fun, that’s what I’m going to focus on. Not this other stuff that’s going on over there.
But give yourself permission to have this be a messy process because it is and do it imperfectly because you’re going to, because everybody does. It’s going to take a while, because it took a while for all of us with this to get there. It’s going to take a while to unravel it. And then even after you unravel it, it can still come back. I still have to watch for this one. If I get triggered with something that is a really high-level item for my OCD, I have to work on this sometimes too, because it’s easy for me to sink back down to this because I did it for so many years.
Kimberley: Which I’m so grateful that you share that because I think that for those-- and I want to make sure I just did it before we finish up and I want to hear about what you’re up to these days is, the treatment for this is actually similar to the treatment of just depression too. You’re working double shifts here, but in a good way. You’re working on two things using the same tool. So, do you have any feedback on that?
Shala: Yeah, that’s a really good point. I hadn’t thought about it like that before, but it’s very much a behavioral activation approach. Behavioral activation is used in the treatment of depression to help people start to put activities back in their lives that gave them pleasure and that gave them some feelings of mastery. And that’s what we’re trying to do with the added component of “And let’s focus on that pleasure. Let’s focus on that feeling of mastery. Those other feelings are going to be there, but let’s focus on the way life used to be before the depression came in.” So, yeah, it is a very behavioral activation type approach here.
Kimberley: Oh my gosh. I love it so much. It’s so good. I feel like everyone needs to be trained in this specific area because it’s such an important area that gets missed and missed and missed and missed. So, you’re like brilliant, brilliant in my mind, as you already know.
Shala: Well, thank you very much.
Kimberley: Okay. Is there anything you want to add before you tell us the way we can find out about you?
Shala: I don’t think so. I think we’ve covered everything.
Kimberley: Okay. Tell us where people can hear about you, your blog, and all the amazing things you’re doing.
Shala: They can go to shalanicely.com. On that website, you can sign up for my newsletter, which is called Shoulders Back!: Tips and resources for taming OCD. I send it out every couple of weeks and it has some sort of new resource I’ve created or been a part of every time I send it out, free resources to help people learn how to effectively tame OCD and reclaim their lives. So, that is where you can go. If you want to read more about this, this particular blog is on my Psychology Today blog. It’s called The Subtle OCD Compulsion that you might not know you’re doing. Again, you can go on my website and it’ll link back to all the Psychology Today blogs as well.
Kimberley: What about your book?
Shala: Yes. So, both books, Is Fred in the Refrigerator?: Taming OCD and Reclaiming My Life and Everyday Mindfulness for OCD: Tips, Tricks, and Skills for Living Joyfully, which I co-wrote with Jon Hershfield. You can learn more about those on my website or on Amazon or anywhere that you buy books. They’re both available on audiobooks as well.
Kimberley: Right. Let me do a plug for your book because I have had so many of my patients say it’s the first time they wanted to hand their book to everybody because it was exactly how it felt for them. I have so many clients who bought a copy for themselves and a copy for their parents because their parents were like, “Oh, this is what it’s like to be you. Now, I finally get it.” So, I’m so grateful you did that beautiful book.
Shala: Well, thank you. That’s the whole reason I wrote Is Fred in the Refrigerator? because I wanted people to understand how it feels to have OCD. If you have OCD, I wanted you to understand that you’re not alone and that there is hope that you can get better. You can tame OCD and you can reclaim your life.
Kimberley: Right. Oh my God, thank you so much for being on today.
Shala: Thank you so much for having me. It was fun.
Kimberley: Such important information. I can’t say it enough. So, so important that we’re addressing this more. I think that this can open it up to everybody having a better understanding.
Shala: Thank you again.
Website: shalanicely.com
Is Fred In the Refrigerator: https://www.amazon.com
Everyday Mindfulness for OCD: https://www.amazon.com
-----
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 194.
In today’s episode, I had the most amazing conversation with Hayden Dawes. Now, Hayden Dawes is a therapist, a PhD student. He is what he calls an “aspiring compassion warrior” – we talk about in the interview what that means. Hayden is just doing some really cool work. As I share, and we go into detail in this episode, he’s really brought out some stuff for me as I’ve watched him and learned from him. It’s been incredible to see this journey that it’s put me on.

So, I cannot wait to share this episode with you. We’re talking about radical permission, writing compassion slips for ourselves. We’re talking about being petty. It’ll make sense when we get there. It’s just such a beautiful conversation. So I’m so happy to share this with you.
If you haven’t already, please do go and leave a review. The reviews help us reach more people and gain the trust of more people. So, go ahead and leave a review wherever you listen, and let’s get onto the show.
Twitter and IG : @hcdawes
Website: hcdawes.com
FB Group https://www.facebook.com
NEWSLETTER: https://www.hcdawes.com/newsletter
-----
Kimberley: Okay, welcome. I’m actually so excited to have this conversation. This was a really, really great one to me because I have with me Hayden Dawes. He is an aspiring compassion warrior – which I can’t wait to hear more about what that means – a PhD student. He is a social worker and has been practicing for many years. So, thank you so much for coming on, Hayden.
Hayden: I am so excited to be here, no one else can see us, but to see your smile, just to see a little of me. That just makes me even feel more welcome and more excited to be here. So, thank you.
Kimberley: Yeah. I’m really excited. So, let me fan go on you for a second. For those who don’t know, and you’ll hear all of Hayden’s work, Hayden has these really cool Instagram profile. I love the work you’re doing with compassion, but we’re also going to share a couple of other things that I love about your work. We’ll talk about that here very soon, but tell me about the work you’re doing around like an aspiring compassion warrior. Tell me what that means and how you are putting that out into the world.
Hayden: Yeah. So, one of the things, I was raised in the Catholic church and Roman Catholic, and I’ve looked for different faith traditions, things that felt close to me and really fit my experience. So, stumbling upon Buddhism and more contemplative practices like Quakerism and Buddhism, and finding the idea of a Bodhisattva, someone that is willing to just do the tough work of delving deeply into what it means to be human, the suffering piece to it, and learning from that experience and then trying to help others along the way as we’re all on this human journey. So, I said, “Bodhisattva is a mouthful. Why don’t I call myself a compassion warrior?” And part of that is delving deeply into my own stuff, my own pains, and challenges so that I can learn more about myself and be compassionate with that and I can be compassionate with other people.
Kimberley: Yeah, respiring. I actually think you’re a warrior. I don’t think you’re aspiring. You could drop the aspiring.
Hayden: It’s interesting. Sometimes I do, sometimes I don’t. It’s like, I think part of the journey is like, “Am I really aligned with that completely? What does the aspiring mean?” Sometimes taking it out of like, “Let me hold closer to this idea that this is what I am.” So, I think that’s influx too, but I appreciate that.
Kimberley: Yeah, of course. Okay. So, we talk a lot about compassion here on the show, but I love those little twists that you bring into it. So, I’d love if you could share, you’re often talking about the permission slip. Can you share it with everyone, for those who don’t know what that means? Can you kind of give me a little rundown of what that is?
Hayden: Yeah. So, back in 2018, I had a friend of mine share on Instagram, a haiku a day for 100 days. I thought, “I’m not counting out all of those syllables.” But what I can do is following up on the work of Brené Brown. I was like, “I can write a permission slip to myself a day.” I can slow down and center myself and think, “If I think about the whole day that I’m going to have, what is it that I most need? What is the thing that I might need to give to myself?”
I also know from my clinical practice, and I’m sure you can relate to this, people will come in and they’ll say, “I’m thinking about doing this,” or “I’m thinking about doing that,” and like, “Sweetie, let’s slow down. You probably know exactly what you need to do.” “What do I do?” I’m like, “Yeah, you’re looking for me to give you permission to do that.” So, I thought, “Well, what if we can just skip through that step?” What would it be like for me to start a practice that I was like, “I’m going to offer myself this permission to do whatever that I might need in the world for myself.”
Kimberley: Why do you think people need permission from other people first?
Hayden: Yeah. I think there’s a lot of different factors, but I think we have a lot of different noise, societal noise about who you’re supposed to be, who you’re supposed to love, how you’re supposed to walk in the world. I think some of that noise trickles into our family spaces. A lot of us are taught to really trust our own intuition, our own inner guide. I might even argue the God that lives within us. So, we end up delegating that task to someone else because we’ve been practicing that, rather than really slowing down and listening and honoring the wisdom that dwells. I believe in each and every one of us.
Kimberley: Okay. So, I love this, and I think that’s so important, particularly for my community who have a tremendous degree of anxiety. They’ve sort of lost touch with their own guide and their own wisdom because fear runs the show all the time. And I think that’s true for anybody who has fear, but especially the folks who have an anxiety disorder. So, I love that. Okay. So, can you walk us through? What would you do? What do you say like WWHD (What would Hayden do)?
Hayden: Yeah. If I’m feeling really anxious, maybe my permission slip is, “Hayden, give yourself permission to just breathe.” Or if that feels like too much, “Hayden, give yourself permission to feel your anxiety. Hayden, give yourself permission to feel your feet on the floor. Nothing else, nothing more, just feet on the floor.” If your anxiety and sort of the thing that you need, you know you need to do is have that tough conversation. “You know what, I’m going to give myself permission to be assertive and to ask for exactly what I need.”
Kimberley: Yeah. I love that. So, it’s in that compassion realm. It’s got like the real boundary-setting one, but also the gentleness. So, there’s both those pieces to it in many situations. I know on, I think Twitter, on Instagram, you post these. Are these ones that you’re writing because you really needed to hear it yourself, or is it that you had a session with someone and you wanted to put that out for other people? How do you do it?
Hayden: Yeah. What a great question. Honestly, all of my permission slips that I’ve written are generally for myself. I want to think that is what connects with people. They know I’m not a phony. They know I’m not trying to sell them some program that I’m not trying to work myself. I have not scheduled any of my posts really thus far when it comes to my permission slips. So, the ones I put on Twitter and oftentimes the one I put on Instagram, sometimes I’ll pull back an archive of what I did in 2018, just to show people that I too am on this path, because I do think throughout my day, like, “What is it that I need?”
Oftentimes with me, and I’m sure many of your listeners can really understand this, that I am someone that does a lot. So, if anything, I need a lot more like parasympathetic energy, giving myself permission to rest, giving myself permission to foster self-love and self-acceptance. But then there might be some people that your permission slip might be a little bit more of like, you need to get up poo and you need to go.
Kimberley: Exactly. I know it’s true. It’s true. As you were saying that, I mean, my permission slips, I could write them for the next month. It would say, “I give myself permission to rest.” I know it’s going to say that, but there are other people who will need for the-- they’ll probably be able to recognize that their permission will need to say like, “Face your fears and do the scary thing.” So, that’s beautiful.
Hayden: Yeah. So, just to give you a little bit more of the story, I didn’t know how much of a big deal that permission slips would be to my work until I was meeting with someone that was helping me to think about my social media a little bit with more strategy. She said, “Hayden, these permission slips are really cool. This is something that I think I could do,” my friend, Emily. And I was like, “Really? I didn’t see it.” That was maybe two or three years ago.
And then what happened was, last spring when I felt like COVID was making our world so much smaller. I was talking to my therapist and she was saying, one of the themes that kept coming up was this sense of reminding people the autonomy that they have. And so one big facet of this is permission slips remind us that we have the ability to choose. Even if you decide not to do that thing, it’s so much more empowering to recognize that you’re choosing not to do that thing.
So then what happened was, I said, “Well, what if I open the permission slips for 14 days on social media?” My following was much smaller than it is now. I did it for 14 days, just how powerful it is to have a collective practice of people all over the world, all over the country, writing permission slips, because there’s something so magical in that by you seeing me give myself permission. It’s contagious. You then give yourself permission.
Kimberley: I agree. I think that’s why it’s so powerful, right? It’s interesting because-- and I hear people say this to me often too. I think people see therapists like, they’re got it all together, which I most definitely do not. I’m not afraid to admit it. I’m totally fine with that, but I still am shocked. I tell people, I share my story because we’re going to break the stigma that therapy is like this idea that you just get better kind of thing, like we’re still so human. I love that you’re a therapist sharing it, because I do think it helps people to recognize like, “Oh, that’s not the goal. I’m not supposed to be perfect. I’m going to be giving myself permission forever.” I love that you’re doing that.
Hayden: Yeah. It reminds me of-- I don’t know, I was jabbering about something with my therapist. She was like, “Are you trying to hack the human out of this process?” And I was like, “I’m trying to hack the Hayden.” It took me weeks later. I was like, “Gosh, she’s so right. I’m trying to do this without feeling any discomfort.” And that’s not going to be possible. How beautiful is it that I can practice giving myself permission by practicing self-compassion literally for the rest of my life.
Kimberley: Isn’t that beautiful?
Hayden: Yeah. I don’t love it, but it’s beautiful.
Kimberley: It is beautiful. I actually have a book coming out on self-compassion for--
Hayden: Congratulations.
Kimberley: Thank you. Yeah. It’s not out yet. It’ll be out in October. But a big piece of it is, if you can hold space for your pain, you’re sad because you will have pain. We’re not going to avoid it. But if you can always be that frontline person, that’s what these permission slips are, right? It’s you being at the front line.
Hayden: Oh my gosh, I love what you’re saying. Now you’re making me think. If you hold space for your pain, you hold space for everyone else’s. I think so much of the inner work really brings out an outward change. You feel so much more connected to the people in your life, maybe it’s your children, your partner, it’s your boss. And then you see the world just so much differently and you see yourself differently and you stop looking at other people’s thinking. Like you said, they have it all together and they live these beautiful airbrushed social media lives. It’s like, “Oh, we’re all trying to be a part of this world and figure it out.” And no one is ever done. If they tell you’re done, I got this for you. They’re lying.
Kimberley: Well, they’re completely in denial.
Hayden: Right.
Kimberley: Right. It’s so true. So, I think I love that you’re giving this very simple but impactful tool. So, thank you. It’s so cool. It’s so, so cool. I have one more question about that before we move on to the other piece of the work, which is, do you actually write them out? I mean, you do because you’re doing it on social media, but I know with Brené Brown, she has had-- you can actually write the permission slip, like it was like, you’re getting a permission slip to leave school early from your parents. Do you write them? Are you now at a place where you can just stop and think it through? What has been your progression with this?
Hayden: Good question. No one’s ever asked me that. So, for me, I generally write them and I think that has been a good practice for me to slow down and stop. But I had a conversation with a friend who has been writing his permission slips, and he said that he’s noticing that he’ll fall into giving himself permission. And then later he can say, “Oh wow, I just allowed myself to do that.”
Kimberley: It’s just a new habit.
Hayden: Absolutely. I really have to sit back and reflect on that to think about, what are the times that I’m just allowing something to happen that I generally wouldn’t have allowed to happen before in the past?
Kimberley: Right. Oh, I love it. I do. I really do. I really encourage people to go and follow you because I do think it is-- even though I know it’s perfect for us and it’s ideal for us to be doing it on our own, I do think it’s lovely to have it be modeled for other people. I think that that’s really powerful.
Hayden: Oh, I have to jump in. I think for me, if you think-- so I actually had a class assignment where I had to really conceptualize what I think radical permission is. Honestly, I think there’s three levels to it. It’s nested within a community. And then the community has an instructional leader. I think of myself as that leader, as someone that is modeling both how to do a permission slip and also modeling how to support others with their permission slips. And then the final component of that is the self-practice.
Kimberley: Right.
Hayden: But one piece can exist without the other. If not, to me, I don’t think it’s radical permission. It’s just not. We don’t exist in containers. Some of the more Western mental health practices, especially in the last 30 years, are so individually focused.
Kimberley: Yeah. I know I’ve got goosebumps listening to you say that because it is so true, isn’t it?
Hayden: This is a community endeavor. I think that’s one of the elements of what makes it radical.
Kimberley: Yeah, I agree.
Hayden: But yet, one of these components can exist without the other.
Kimberley: Right. It’s the unlearning, isn’t it? Right? So, as a child, if you’re in an environment that doesn’t support this kind of work, if you’re in an environment where there are people, it is the unlearning of that. It’s so important.
Hayden: Yeah. And the unlearning, I just want to validate for people out there, is so exposing, so vulnerable, so raw.
Kimberley: Right.
Hayden: When you push someone trying to help you experience your own power and your own sense of autonomy over your body, your thoughts, and your ideas, and then your behaviors from that, wow.
Kimberley: Yeah. It is. It’s funny. I love when I have these teen clients and we’re talking about a concept. I can see them shaking their heads and they’re like, “Nope, nope, nope. Not going there with you. Nope. No, thank you.” They’ll roll their eyes or something. And then upon second and third conversation, there’s a body shift for them. I’m like, “Really? I can do that? Really?” Interesting, right? And then there’s a total body shift. I think, I mean, I’m just so grateful you’re doing this for people all over the world. So, it’s very, very cool.
Hayden: Thank you.
Kimberley: Yeah. Oh my gosh. Okay. I’m so geeked out right now because I love compassion, but I just really cannot wait to talk to you about this. I’m so curious--
Hayden: You can hear me fumbling around this. I just want to put that on the table.
Kimberley: I’m going to fumble too because really, I don’t-- let’s just fumble together. Right? I follow Lisa Renee Taylor and she always says “Stumble bravely.” And so I’m like, “Yes, let’s stumble bravely.”
You on your Instagram have Petty Tuesday. Now, I’ll be totally open with you. The word “petty,” I had this visceral body experience. When I first saw this, I was like, “What is he doing?” These were like petty because in my mind, “petty’ just had this connotation to it. I think again, it’s the unlearning, right? It’s the unlearning of like, “What, wait, we’re going for petty? What’s he doing now?”
Hayden: Oh my goodness.
Kimberley: But now I’m hooked on it. I love it. I can’t get enough of it. And that’s the thing, right? It’s the unlearning. So, let’s just go from the start. What is Petty Tuesday?
Hayden: So, something was happening in the national headlines and I was just like, “Really? come on.” It was like hearing about one of these talk show hosts having a really bad, toxic culture. I was like, “What on earth?” And so I just started talking on my stories about it. I literally would talk about it with my friends like, “This is a really messy situation. People are being harmed and people are being hurt.” I was like, “Not to be petty about it. I mean, Petty Tuesday.” And then people started DM-ing me and laughing about the fact that I said “Petty Tuesday.” So then I just started incorporating it because I honestly started having fun with it. It feels really playful.
Kimberley: It is.
Hayden: It’s interesting because I looked up the word “petty” and there’s all these different definitions. But the one that I really like is, it’s childish. It really is childish. It’s playful. It’s an opportunity. It’s an invitation not to take ourselves too seriously.
Kimberley: Yeah. You see, this is why I loved it. So, I have a Buddhist training too. I’ve really been working for many, many years – I had an eating disorder – since my recovery on, like trying to read petty. We don’t want petty, right? We don’t want to engage in too much anger because that’s got its own pain and suffering with it. Not that I’m saying any of these things are bad, but then you’re totally leaning in over here.
Hayden: Yeah. I think the sort of idea of toxic positivity and how broken that is, and I think there’s some wisdom about honoring our pettiness. not honoring it to be fixed to it, but to realize that there’s space for it, because you either acknowledge you’re petty or your petty will really rein you.
Kimberley: Yup. I just love-- so the reason that this showed up for me and there was a shift for me, like I said, there was a three minute, like, “What is he doing over there?” And then it was like, “Wait, what he’s doing is he’s practicing non-judgment.” And now I’m watching every Tuesday and then people are posting their petty things, and I’m just like, “This is so great.” We’re having an emotion and we’re not going, “Oh, that’s so bad. I shouldn’t be feeling that way. What’s wrong with me?” and all the things. We’re just going, “Yup, it’s petty Tuesday. That’s what we do.”
Hayden: Yeah. I think there’s something about the discipline of doing it on one day in particular that I have some people-- honestly, I completely stumbled, well, not bravely, but I stumbled into this, and now everyone’s like, “Oh my gosh, I love Petty Tuesday.” I will be honest, sometimes it’s become a piece of, I’ll use a term “brand” that I’m like, “People really like this?” but like, “No, I see myself differently than this. I see myself cross-legged on some mountain.” But everyone’s like, they’re feeling seen by it. It’s not--
Kimberley: I think it’s the opposite of the position. The permission slip, when I think about it, that might be why I’m hooked because, on the permission slip, you’re giving permission to do this beautiful thing. With Petty Tuesday, you’re giving yourself permission to be around emotions that we would usually disavow. You’ve just got this whole spectrum going on.
Hayden: You are articulating some parts of my process that I have not quite figured out yet. How much do I owe you for this session?
Kimberley: No, actually, I’m trying to figure it out myself, right? Because this is why I really think, okay, so I’m a consumer in this perspective. So this has been learning for me. And even noticing in myself like, “Oh, isn’t that interesting?” My first reaction was like, people can’t see my hand over my-- petty.
Hayden: It’s taboo.
Kimberley: Yeah. Like, “What are we doing here?”
Hayden: Yeah. I think part of it is, being a gay man, it’s like, pettiness and kind of cattiness, that’s what the stereotype is of gay men. Yet, it’s part of our culture. I think there’s this idea of why folks love RuPaul’s Drag Race is because it leans into the non-seriousness of living and how really a lot of these constructed boundaries about what’s okay to do and what’s not okay to do is socially constructed. So we have to socially deconstruct them, or to use your term, unlearn them.
Kimberley: Right. I love it, and you do it so well. And this is why I love it, because if I think I did Petty Tuesday, it would just be like a venting session. It wouldn’t look the same.
Hayden: Well, yeah. I mean, it’s interesting. I was going off about a celebrity couple that got back together. And then later, I felt guilty about that. I was like, “You know what? I felt like I went too far with that.” But this is where the compassion works, is helpful. It’s like, yeah, that might’ve been a tiny bit mean-spirited, but in the big scheme of things, it’s not that big of a deal. Also, it’s like, it’s been so transformative for me to recognize that I can use my voice and the power of my ability to communicate. I might hurt people, and there are times that I have hurt people in my past. But wow, does it feel great that I can be accountable to my word and say, I’m sorry? I often think we wouldn’t need a cancel culture if we allowed more space for radical accountability.
Kimberley: Yup. I agree. No, I’m loving it. Don’t change a thing. Don’t, because I think it’s beautiful. I’m really in love with it because again, I think that even from the anxiety-- the work I do, let’s actually look at, you said toxic positivity, it’s so important to address that. I had a lot of this in my childhood. We don’t do petty. We don’t do angry and we don’t do those other things. So, I’m loving this idea of like, I can make space for all of the feelings and I can also just embrace the humanness that is petty, because I don’t think everybody’s thinking petty.
Hayden: Yeah. This morning I went to the gym. This is my petty thought of the day. okay, so the gym has music you can hear throughout the whole gym space. And then you have folks that are walking around with their phones on speaker phone so that you can hear their music, like it’s their own private boombox, and I’m like, “Isn’t that what headphones are for?” And I’m like, “Oh my goodness, whatever. Okay.” But in the grand scheme of things, this is a first-world problem, but the pettiness of me is like, “Come on now, boo.”
Kimberley: Right. So I’m liking this. This is what I’m saying. I was just actually about to say, give me your petty of the day. Yes. And my petty is probably more related to my children. I’m like, “Do I have to say it 12 times? Do I have to put your left shoe on? Come on.”
Hayden: Well, can I ask you a question?
Kimberley: Sure.
Hayden: I hate it when people are on podcasts and they’re like, “Can I ask you a question?” That’s a pet peeve of mine and a petty, right? Like doing it after going through your petty process about, with your children, what does that do for you?
Kimberley: Well, I actually did a post on this, this week because I’ve actually been really working through my relationship with venting. I think this is why-- if I were to really look into it, you probably started this work I’m doing.
Hayden: So you owe me [28:45 inaudible].
Kimberley: I do. We’re actually even at this point, so we’ll balance the sheets out at the end of the session. But I think that it probably was. If I really think it was probably spurred by this, it’s to start to reflect on, when I open up space for this, like, I don’t want to call it a negative emotion because it’s not, but just for emotions that bring up some suffering for me, right? My instinct is to shut it down. I think what that means is it shuts down, it shuts down, it shuts down until I cut to the point where I need to vent. By that point, the boiler has gone and it’s coming out. So, I’ve been working better instead of holding space for the petty. So I don’t have to vent. I don’t want it to get to that place. Not that there’s anything wrong with venting either, right?
Hayden: I love what you just said. I’m really going to slow down and hear that because I think what it brings up for me is-- a lot of our somatic practitioners would tell us that we need the energy to keep moving. Really pettiness is just another form of energy. It’s not good or bad. It’s just another form of energy.
Kimberley: Right.
Hayden: And I think what you’re saying is, and what I’m hearing is like, let’s open up the space to let the energy keep moving, so that way it doesn’t become locked up like a dam, so that when it gets so full-- because I think the issue with that is it can get so full and burst. And then it starts this whole cycle of filling the shame and filling the guilt of a complete eruption.
Kimberley: Right. Exactly. So, if I step into my petty, it doesn’t feel good because of the learned judgment on that. But it’s me learning. I’m learning that if I can stay with the feeling of that – it doesn’t feel good, but it also feels good – it will save me from really not feeling good when I go into vent mode. And so for me, it’s been really-- like I said to you, I just love it. I do. I really do. I think it’s beautiful as long-- I think that the conversation we actually had on Instagram, because I did a post on this was, people’s conversation around like, but you can’t take that away from me. Really I’m at a stage in my life where I need to be a lot petty or a lot venting. I think for people, it’s different.
Hayden: Absolutely. Yeah. Thank you so much for sharing.
Kimberley: Oh, of course. Thank you. So, do you have bigger petty days than other days? What’s the influx of petty for you?
Hayden: I don’t think of myself as a petty person. It’s interesting that I have an experience. I think being an immigrant and being a military child and accepting life as it is, a lot of acceptance energy of things that other people might complain about is part of my story. So, I think there are days where I may have to lean on my petty and get a little bit more. But that’s anger, which feels a little bit different for me. Yeah, I might feel a little bit aggravated a little bit more often some days compared to others. It’s not something that I necessarily am probably the most tuned into. So, you’re offering me an invitation to think about that a little bit more and to contemplate on it.
Kimberley: I love it. Okay. So, is there anything that you feel like we’ve missed here? We’re stumbling bravely. Do you feel like there’s something about Petty Tuesday, the concept of being petty for people that they may want to consider as they move into embracing this?
Hayden: I think the thing that’s really important to know is that it’s vulnerable. Even being petty is vulnerable and allow your pettiness, allowing yourself to come out to your own inner pettiness because you’re unlearning something and you’re trying something else that you’ve never tried before. So, it’s going to feel scary, especially when you’re riding the wave of a new emotion. You don’t know what’s going to come out. You don’t know who’s going to come out on the other side of it. So, I really want to validate and normalize all of that. I do think there needs to be some safeguards on the other side. There’s a difference for me between pettiness and mean-spiritedness and complete toxic negativity.
Kimberley: Okay. That’s helpful to hear. Yeah. How do you differentiate that?
Hayden: Pettiness has a playfulness, for me. I think the playfulness, again, not taking myself too seriously. When you think about children playing and you think of yourself playing, for me, it’s a wide-open field of discovery and mean-spiritedness. The energy just feels like a dark cloud or there’s a monster and it’s like, “Ooh, I don’t really like that energy. I’m not judging it. I’m just saying I don’t really want more of it.”
Kimberley: Right. Yeah. I mean, I think that there’s a small shift in that it’s intended to create harm, right? It’s intended to displace whatever you’re feeling kind of thing. I can feel that too. I think that that’s a really good differentiation. I just love it, though. I can’t help it. I just laugh when I think about it.
Hayden: I mean, you’re smiling about it.
Kimberley: Yeah. That’s not it. It’s so perfect.
Hayden: There’s something fun about it. People look forward to celebrating Petty Tuesday. People are like, “Hayden, please create merch so I could wear a Petty Tuesday t-shirt,” and I’m like, “Oh my gosh.”
Kimberley: You totally should. Yeah. Again, I think it’s one of those important lessons that we have to unlearn, which is, there isn’t really an emotion you can’t touch on. Maybe that for those who are new to this day, permission slip could be, I’m going to allow myself to feel some petty.
Hayden: I love it.
Kimberley: Play with that.
Hayden: Absolutely. I think so much of unlearning and learning something new is play. giving yourself space to try it out. Commit to it and try it out. Yeah. Permission slip to be petty or to be aggravated. I mean, one of the permission slips, and this is a different emotion, that has completely changed my life was right after the murder of George Floyd, Ahmaud Arbery, Breonna Taylor. I wrote permission slips to myself to channel my anger to rehumanize myself in the midst of dehumanization. I did not recognize the connection.
But after that, I wrote this piece that went viral in the therapist community called An Invitation to White Therapists. It’s completely changed my world. It’s got me in conversations with mentors of mine, people that have huge followings and are famous in my world, because I gave myself that permission and to really, really experience and feel that emotion and to trust that my container, my nervous system, that my body could hold whatever might come out on the other side. I definitely think having relationships that are there to support you in your play of discovering who you might be on the other side is really important and fostering that. That’s made all the world of difference to me.
Kimberley: Yeah. I thank you for sharing that because I really do resonate with that as well. Feelings are scary. I think that we don’t give ourselves permission because we don’t want to feel what could come with that. Particularly around those conversations, those very difficult topics, I think it’s so important that we slow down, maybe write out a permission slip first. I know I have to do that all the time with social media areas. Okay, how do I navigate this conversation? Can I be okay with it being imperfect?
Hayden: Yeah.
Kimberley: Yeah. Thank you. I’m so grateful for you bringing that up because I think that’s amazing. Okay. I actually have one more question for you and then I want you to tell people. So you’ve said when we were pre-having this conversation that you are a curator of radical permission, what is that?
Hayden: Yeah. I have to be honest. Some of this is based on Rising Strong process, a Brené Brown book, but I do think I’ve moved it forward in making it a collective practice. So, I think of myself as the curator because, do I own this? I think our Western way of we own things, like, do I own this? No. If anything, I feel like more of the shepherd of it. I hope that this lives beyond me, honestly.
So, I think I love the word “curator,” thinking about someone that is there to be a custodian of a space and of a process and there needs to be some editing. So, there has to be some power that I hold of the process because you need to make sure that it stays within the pathos and the ethos of really what the values are underpinning it. So, I think that’s why I use the term “curator.”
Kimberley: I love it. Okay. Tell us where people can hear about you. I’m so grateful for this conversation. Really I am. I could literally talk to you about this for hours, but I’m not going to take your time up. Tell us where people can hear your stuff and learn well from you.
Hayden: Yeah. So, you can follow me @hcdawes on Twitter as well as on Instagram. There is a Radical Permission Facebook group that you can search. You can also head to my website at hcdawes.com. I also have a monthly newsletter where I talk about all the things that are important to me, and I hope it offers you value. I always offer something for you to contemplate about your life, as well as there’s always a petty moment, as well as different trainings that I’ll be offering and different upcoming events.
Kimberley: Yeah. Thank you so much. Like I said, absolutely just grateful for you. You’re doing amazing work.
Hayden: Thank you.
-----
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
This is Your Anxiety Toolkit - Episode 193.
Hello, my loves, how are you?
So, recently, I’ve been having lots of conversations with my patients and my clients around one really helpful metaphor around managing mental compulsions.
Now, before we go into this, let me just do a quick overview. We have obsessions, which show up in the form of intrusive thoughts, intrusive feelings, like anxiety and uncertainty and doubt and guilt and disgust. There’s intrusive thoughts, there’s intrusive feelings, there’s intrusive sensations, which is whatever physical sensations you experience that are intrusive and repetitive, and then intrusive urges. Urges like this urge – you feel like you’re going out of control and you’re about to hurt someone or you’re about to harm someone or do something that is ineffective or not helpful in your life.
We have these intrusive thoughts, feelings, sensations, and urges, and sometimes images as well. It might be a quick flash image of something scary. In effort to either solve that or remove that or lessen the discomfort of that, we engage in a compulsion. Now, the compulsion could be physical, like washing your hands or moving an object or so forth, checking something, or it can be mental. I’m really specifically, in this episode, talking about mental compulsions – the mental compulsion of trying to solve and ruminate on an obsession. A lot of you have said that mental compulsions are one of the most difficult to reduce or prevent or stop, and I think that’s very, very, very common.
When I’m talking with my patients about this, usually, they report that once they have the obsession, because we know that – let’s sort of just preface – trying to prevent the thought or suppress the thought won’t work. You’re going to have these thoughts. Thoughts suppression usually makes you have the thought even more.
We’re not talking about thoughts suppression here, but what we are talking about is, once you identify that you’ve had the thought, how much attention do you give it and how much leash do you give it? This is the metaphor I want you to think of.
When you’ve had this intrusive thought, think of the thought like a really baby puppy, like a really active bouncy baby puppy, and you’ve got the baby puppy on a leash. You’re taking the puppy for a walk.
Now often I’ll ask my patients, “When you take your puppy for a walk, particularly if you live in a suburban or city area, which I do, do you give the puppy a long leash or do you give it a short leash? As you’re walking down the sidewalk, are you letting the puppy walk down the middle of the road with a long leash, and then it jumps over the sidewalk into the garden, it pees on the garden and then wraps its leash around your legs, and then it takes you off into some at the park that you don’t want to go into? Does it walk down a street that you don’t want to walk down? Or do you keep the leash shorter? And what you’re doing there is you’re pulling it back. You’re not allowing it to go into areas that you don’t want it to go.”
Now, that’s what I want you to think of in regards to mental compulsions. Once you know that you’ve had an intrusive thought, your job is to keep that thought on a short leash, meaning you don’t explore the whole neighborhood and what it means and what it could happen, and this could happen, and that could happen, and let’s go down the rabbit hole of trying to figure this out. Instead, you want to keep it on a shorter leash. Again, in this case, you’re being really skilled in what road you’re letting yourself go down or what rabbit hole you’re letting yourself go down. The whole idea here is, keep your intrusive thoughts on a short leash.
You still have the dog. You’re not trying to get rid of the dog. You’re not cutting the leash short and going, “Runaway, I don’t want you.” You’re saying, “I have this thought. It’s going to be here. I’m going to be very intentional on where I allow this thought to go. I’m going to be very intentional on how much I let this thought be the focus of the walk I’m taking.”
As you’re walking your dog, you’re not only looking at your dog. You’re also looking at the path that you’re walking on so you don’t trip. You’re looking at the nature around you. You’re waving to the neighbor or however. You’re engaging with the outside world. You’re not just gripping and holding the leash and fighting it.
This is important for you as you manage your mental compulsion. I’m going to say to you, this may be the most important skill you’ll learn. The skill of managing mental compulsion is so important if you have generalized anxiety, OCD, social anxiety, health anxiety, depression. It’s so important that we are skilled at setting boundaries with our mental compulsions or our rumination and our worry. All of these things are the same. Worry is just a form of mental compulsion.
What we want to do is, if you notice that you’re going way down the wrong street and you’re going in the direction of doing mental compulsions, you may want to yank on that chain and say no, as you would with your dog. “We’re not going down that street. We don’t poop in people’s yards. We don’t poop in our own yard. We stay on the sidewalk.” And then the dog tries to go the other direction into that person’s garden, and you say, “No, sorry. We’re not doing that today. We’re staying on this path. You can be here. The thought can be here, but I will not let it determine what I do on my walk.”
This is so important. Just think of it. Think about when you’re in your daily life, do you allow your thoughts to be on a tremendously long leash and do they go wherever they want and they’re pulling you in every direction, or are you in the practice of shortening that leash and taking more control over where you let your head go?
Now, a major thing to remember: It’s entirely okay if you suck at this. You are going to suck at this. Please, don’t be hard on yourself. This is a practice. There are some days I am excellent at this. There are some days I am terrible at this. That is okay. It’s similar to anything in your life. You’re going to have ups and downs. But really reflect as often as you can, what’s the intrusive thought, what’s the intrusive feeling, sensation, urge, image. That’s the obsession. We don’t want to control that, but we do want to work on being skilled at how we respond. That’s the most important piece.
Be gentle. Be kind. Be diligent. Be patient. You will get this with time. Keep that dog on a shorter leash, if you can. Be gentle with the puppy on the leash too. Don’t yank on it too hard because we don’t want to get into a wrestle with our thoughts. Okay?
I love you. I hope that is helpful. Please, please let me know your thoughts on this. It’s just a metaphor, so it may be helpful for some and some maybe not for others. I just am so grateful that I get to spend this time with you.
Please go and leave a review. I know I say it every single time. I cannot tell you how much it helps me and brings me so much joy to see the reviews. I love them. Thank you so much. I read every single one. Thank you. We will give a pair of free Beats headphones to one lucky person who leaves a review as we hit a thousand reviews.
Thank you so much. I love you, guys. Have a nice walk, my friends. It’s a beautiful day to do hard things.
This is Your Anxiety Toolkit - Episode 192.
Welcome back, everybody. I am really excited to do this episode with you. It’s a little bit different to episodes I’ve done in the past, which might be why I’m really excited about it, but it is a skill I have been practicing for several months. No, maybe more than that. I would actually say closer to six months to a year, and I was reflecting on, what are the things that... I took a lot about mindfulness skills and a lot about therapy skills and cognitive behavioral therapy skills, but is there something I haven’t really talked about in terms of just lifestyle? And I thought this, of all the topics, is probably one of the things that helps me manage my anxiety and depression the most, literally the most. In fact, I would go as far as to say it has been probably one of the most important things that has helped me recover in my recovery, and I’m really excited to share it with you.
Today, we’re talking about how activity scheduling and managing your schedule can be a really important anxiety management tool. Before you completely sign off and say, “Oh my gosh, this is not for me,” please just hear me out because there is so much greatness to being really intentional about your schedule and scheduling.
A couple of reasons I say that is because, number one, if you are somebody who has a job or goes to school or has a mental illness, and that’s really, really debilitating and taking up a lot of your time, or you have children or all of the above, it’s really easy for the day to just come and go. And before you know it, you haven’t gotten done what you wanted to get done. You’re feeling more and more anxious about tomorrow. You’re feeling more and more depressed about yourself and what you’ve got to do. You’re feeling bombed out because you didn’t get to prioritize your time.
And that was exactly me. Every time I opened my eyes in the morning, I had this sensation of dread because I just was like, “Oh my gosh, today’s going to be another huge day. I’m going to run all day. I’m in a rush all day,” or “I’m going to feel anxiety all day.”
Let me tell you a couple of skills that I teach all of my clients because, as I’ve said before, this is something that they talked to me about, at least once in their treatment, is how to manage their time.
Okay. I have learned and I have practiced this, like I said, for almost a year now – the art of scheduling in a way that is in the intention of benefiting my mental health. I don’t schedule because I want to be super time efficient. I don’t schedule because I want to get a ton done. I schedule for my mental health, literally. Forgive me, if you can hear beeping car alarm, it’s been going all day. So I’m sorry if you hear that in the background.
I literally schedule for my mental health. And what I have learned, I took a whole course on this, is one of the biggest mistakes we make with scheduling is we schedule what we have to do first, and that basically means we’re prioritizing work and school and to-do’s, instead of scheduling pleasure first. So that is what I want you to practice first.
That already might be mind-blowing to you. You might be like, “Wait, what? Like pleasure? That’s important?” Yes. Schedule your pleasure time first. Look at your schedule, even write it on a piece of scrap paper. What do you love to do? Make sure you schedule that something. Even if it’s for 10 minutes, you schedule it every single day.
Once you’ve done that, then you schedule what you need to do for your recovery. It may be different for every person. Some of you may need to schedule exposures, and again, be very intentional. Let’s say you have a driving exposure. You have to go driving for your exposure and practice having intrusive thoughts, or you have to practice going and doing a certain thing that concerns you or scares you. You’re going to schedule that time first.
If you’re not someone who’s doing exposures, maybe you have to schedule time to correct your thinking or schedule your time to meditate. Schedule your time to read your mindfulness book. I have almost all of my patients read some kind of book that will complement their treatment all the time, meaning throughout treatment. Once they finish one book, I send them a book to read after that, and I tell them, “You don’t need to read all day every day.” I might ask you to read a page a day or a chapter a week, or whatever works for you, but schedule that in because really literally, I’ll give you an example.
I have a private practice and an online business, two complete businesses. I’m managing up to 15 to 20 people a week. If I worked at scheduling my to-do list first, I would never take care of myself. Never. I would only work for other people. I would only be doing a million to-do’s. I would never get any exercise. I would never meditate. I would never have any time because I would have just clogged up my schedule with that.
Reverse it. First, schedule your pleasure and then schedule your mental health practices, whatever that may be – your self-compassion practices, listening to a podcast, whatever it may be.
Now, when it comes to the things you have to do, this is going to go against some of the advice you’ve been given. I know it will. But hear me out and you can take what you want and leave what you don’t want. What I do is I sit down with a piece of scrap paper and I write a to-do list. Every Sunday, I do this. I write a list of all the things I need to get done this week. I write a list of what emails I need to write and what phone calls I need to make and what bills I need to pay, and who I need to talk to, who I need to consult with, and so forth.
Now, for those of you who compulsively list-write, we’re not writing things that are daily activities, like I’m not going to write “Brush my teeth.” I’m not going to write “Have breakfast.” I’m not going to write “Lock the door.” I’m not going to write things that I would be doing anyway. I’m going to be writing the things that I have anxiety about and that are important that I get done and that I value. I’m not writing down things that are compulsions or things I’m doing to make my anxiety go away. These are just really logical things that I have to do.
Once I’ve got everything down, I don’t keep that list. I transport that list into my schedule. Of course, I have to see my clients. Of course, I have my clients in my schedule weekly. But then from there, let’s say I needed to make an email to, let’s say my website programmer, I would put that in the calendar. Tuesday at four o’clock or Monday at six o’clock or whatever it may be. I take everything from the to-do and I put it on the calendar.
If you’re noticing now that the calendar is full, something has to go, because what’s happened in the past is you put all the to-do list in, and so the thing to go is your mental health, is your self-care. We can’t do that anymore. That’s why I’m telling you, like, that’s why scheduling is so important because if you don’t, you’re going to realize that there is actually no time for self-care and there is no time for your mental health. If that’s the case, like the whole saying is “Nothing changes if nothing changes.” So this is so important.
You may need to ask for help. I’m always talking with my patients about asking for help. Okay, you need to go out for a drive. You need to do your homework, but you also need to take the kids to school. Can you ask someone to help you? Can you pay someone to help you? Can you find creative ways where you take your kids and someone else’s kids one day and they take their kids and your kids the next day? Again, I really love to do this on the cheap, so I don’t want this to cost you money. Can you find ways to prioritize your mental health in your schedule, on the books, and open up time so that it becomes the priority?
I know I’ve told you this story before about, I was at a lunch and I was with my friends and they didn’t have children. They were all talking about these beautiful hikes that they were going on. I said, “Well, I can’t go on a hike because I have children.” He’s like, “Yes, you can. You just haven’t prioritized taking a hike. If you really wanted to, you would take your kids on a hike or you would find some time or find someone to take care of the kids so you could go on a hike. But you haven’t prioritized that. You’ve prioritized being with your kids or working or taking a bath.”
There’s no judgment. There’s no judgment to what he was saying. He was just saying, “You can do it. It’s just that you have to figure out what is a priority.” For me, that was shocking because I was like, the truth is I say my mental health is a priority, but I don’t. That doesn’t show up in my schedule that way. This was many years ago, and it was a crazy aha moment where I was like, “Huh, I say self-care is important, but it’s totally not evident by the look of my schedule.”
The other thing that I have found that’s so fascinating is, once I started doing this, I started actually realizing how much I was working or how much I was doing behaviors that bring me no pleasure. I spoke with a client about this just the other day, is I wasn’t feeling so well. I went to bed early. I laid in bed. I opened up Instagram. And two hours later, two hours later, I come out of a thick fog of Instagram and realize that I’ve lost two hours. The thing to remember here is, number one, that’s neither good nor bad because some people love Instagram and it brings them tons of pleasure. But in that moment, as I checked in with myself, I didn’t feel any better. If anything, I felt more stressed.
So what I was doing was I was engaging in behavior that I could have done that would have felt so much better and aligned more with my mental health, which again is why I say to you, please, please, please, if you take one thing away from today, please schedule your pleasure. Please schedule your pleasure, the things that bring you joy.
Now, some people say, “I can’t do those because my anxiety has taken those things away from me.” Even more reason to schedule them. If you love to read and your anxiety or your depression has sucked the joy out of reading or writing or whatever you love to do, schedule that and work at what’s getting in the way. Talk with your therapist or journal or try and figure out what’s getting in the way and work at making sure that fear isn’t your scheduler. Fear isn’t your assistant who schedules your day. That’s not cool. That’s not kind to you. Do not let fear schedule your day. Do the best you can is what I should say, because there will be times it will. But just do your best to make a deal with yourself.
We’ve talked about transferring your to-do lists onto the calendar. You rip the to-do list up, you take it away. And then your job is to do your best to stick to the calendar. It’s not going to be perfect. In fact, it’ll be far from perfect, but really look at the end of the week or at the beginning of the week, and look at your calendar and make decisions with that.
Now, of course, I understand that there is some degree of privilege involved here. I want to make sure we respect that some people don’t have control over their schedules, and that’s true for many people. But what I want to ask you is, if that is the case, where you have control, can you implement really good exercises and activities during that time, like really resting.
I just read an amazing book where they were basically saying “Schedule rest.” If you’re someone who’s working a double shift and money is tight and life is really difficult right now, maybe the first step is you just schedule rest. Maybe the only step is for you to schedule rest. Maybe we start really simple. This is a lot of change. I encourage you to take baby steps, even if you’ve got full control over your schedule. It’s really important here that we take baby steps and empower ourselves to prioritize your mental health. Believe me, it is going to make such a change.
The other thing is, and I’ll say one more point, what was really interesting to me is, I really then, once I started scheduling, noticed all the “shoulds.” Well, I should work out five days a week and I should go and help other people, and I should be putting this in my schedule, and I should be calling this person.
As you do this, ask yourself, do you really want to? If it’s not a “have to,” meaning you have to go to work and you have to go to the staff meeting and you have to show up for school and so forth, really check in with yourself. Are the things you’re doing on your schedule because you feel like you should do it, or because you want to do it, or because you have to do it? Be honest with yourself about that, because I found on my schedule a bunch of stuff. I would even say a bunch of swear words, a bunch of crap that I really didn’t have to do. I was only doing it because I’d made up a story about the fact that I should, and it wasn’t even a fact and I was doing it out of fear.
That’s why I really, really wanted to chat with you about this. Easier said than done, like I said, but really think about this. Look at your schedule. If you can – I schedule on Google calendar, it’s free –look at your schedule and ask yourself, is it reflecting the level of recovery that I am wanting?
Make small changes. This is really important. If you’ve learned one thing from today, it’s please schedule your pleasure. Really schedule your wellness. Schedule your rest. Work the rest around that.
Okay. I love you guys. Have a wonderful, wonderful, wonderful, wonderful, wonderful, wonderful day. I believe in you. I believe you can do this hard thing. Do the best you can with what you’ve got. I am so grateful for you spending your time with me and being on this journey with me and taking me along with you. Thank you. I know your time is valuable and I’m so grateful.
Don’t forget to leave a review. I would love nothing more than to get your honest opinions about the podcast. So, please do that, and have a wonderful day.
If you’re interested in any of the resources that we have, go over and look at cbtschool.com. Check it out, and have a wonderful day.
This is Your Anxiety Toolkit - Episode 191.
Well, welcome friends. How are you? How are you doing really? I want you to reflect for a second on just that... on just that question. How are you?
I have not prepared for this episode. I just thought I would sit down and take some time to reflect some of, I’m sure, what I reflect on will be the first time I’ve reflected on it and not just that for reflecting with you.

So what I wanted to talk with you guys about is life with a chronic illness or a disability. This is something that has shaken me a lot over the last, I would say two to three months. A lot of you have the background story with me, but if you’re new here, welcome, and I’ll tell you a quick background.
In 2019, I got very sick. Through that process, I also got very... not just medically, but mentally struggled because of the symptoms that were incredibly debilitating. After pretty much every single medical test under the sun, I was diagnosed with a lesion in my brain, that they still don’t know what it is, and a disorder called postural orthostatic tachycardia syndrome.
It sounds scary and it can be scary, but mostly, it’s a disorder to do with your autonomic nervous system and it basically involves lightheadedness and fainting and headaches and overall exhaustion and nausea and very, very big degree of brain fog. It can be mild and it can be very severe and extreme to the point where you can’t stand up.
For months and months and months, particularly throughout COVID, I have been doing my very best to manage this disorder and this syndrome and have been doing really, really well. I’m not going to lie, I thought I’d mastered this disorder. I really did. I think there was a cocky piece of me that was like, “Oh yeah, look at me.” Once again, hard work pays off. And yes, it does. Hard work does pay off.
But recently, I have been hit with another... I call it an event, another wave of POTS – POTS is the acronym for postural orthostatic tachycardia syndrome – and it has knocked me off my feet literally. Not figuratively. I think both.
For those of you who don’t know, I was, two weeks ago, taking a tennis lesson, a part of my attempts to take care of myself as I have cut back immensely with work. I’ve mentioned my kids are gone back to school and my husband’s gone back to work. And so I really decided, I made a conscious decision to put my mental health first.
I had started taking tennis lessons, and in the middle of my tennis lesson, it was very hot. I collapsed and had to go to the hospital. I’m sorry if this is scary for some of you. It had to be monitored and got IV bags and medications and all the things. Again, once again, I really thought this was a short-term thing.
What I am reflecting on today is the realization that I’m not going to manage this. I’m not going to master it. This is something I will probably have to handle for the rest of my life. I was expecting to bounce back and I didn’t. I’ve had many days of not being able to stand. I’m not able to drive. I can drive on certain days, depending on how busy I am, but I have mostly not been able to drive. I am unable to work out.
I wear these most fabulous compression socks right now, the compression socks I’m wearing. I have bright colors in stripes. I have ones with spots and reindeers and all of the things. So, that’s very fun. But no matter how much I hydrate, I’m struggling to eat and so forth.
The reason I wanted to share this isn’t just to... of course, I can share. I want to share with you. But the main reason I wanted to share with you is to talk about what it’s like to wrap your head around long-term suffering. I’m really interested in this because I’ve been really mindful and watching my thoughts about this syndrome. I wonder if this resonates with you guys because a lot of you are dealing with either. A lot of you have reached out and said you have a chronic illness too, or chronic mental illness, anxiety, depression, or any of the disorders.
What has been really interesting for me is to catch the thoughts I have around disability. now, the first thing – and I’m really open about this, and I’m really happy to share how far I have to go – is I didn’t realize I had all this stigma around the word “disability.” I have a career in people with disabilities or struggles or long-term chronic stuff. I wouldn’t judge anybody else, but interestingly, as soon as I had to recognize, I kept saying, “I don’t know why this happened. I don’t know why this happened. Why did this happen? This shouldn’t have happened.” My doctors said, “No, you’re going to have really big ups and really big downs. That’s going to happen. That is a part of this disability.” I really was able to observe how judgmental I was about that in myself.
The word “disability” was not okay with me, the word “long-term chronic illness.” I was like, “Uh-uh, no way, I will solve this,” until I had to be like, “Wait, that’s a lot of energy, negative energy on something that does not serve me and is built around a stigma and a judgment of me having a disability.”
It’s so painful folks to observe that. Thank goodness I have those skills to be able to go, “Okay. That was judgment. Interesting.” I encourage you guys to take that approach when these types of thoughts come in. Because again, I’m always working with my patients and clients and people on social media around the stigma of the word “disorder” or “disability” or “mental health” or “mental illness.” It’s important that we catch those judgments.
Now, once I caught it, to be honest, I didn’t do much with it because I really just had to hold some space there to wrap my head around, “Whoa, okay. This is a long time for me now.” I thought I was the special one who could get through it and it’s not going to bother me again, but it’s not. It’s going to come back. This one has been particularly painful, physically 100%. This was probably my most serious event or wave of POTS. But also, just to be able to really look at how it has impacted me mentally.
Now, here’s the thing. Once I came to the understanding, not just the acceptance yet, but the understanding that this is long-term and something I have that I will have to continue to manage, it was so interesting how my thoughts wanted to go to hopelessness. “Okay, well, now my life’s going to suck,” or “I should give up. This is going to impact my life and terribly impact my life. This is going to ruin my life,” and so forth.
Again, it was being able to observe and catch and watch myself go into hopelessness and be able to... If you could see me, I would smile and go, “Ah, okay, interesting.” That’s the story I’m telling myself because here’s the thing, I’ve had this since 2019. I’ve been managing it this whole time with the thought “I can manage this.” And therefore, I was happy.
Now, nothing has changed. I’m still having POTS. I had another incident. The only thing that changed was now that I had a recognition of this being a problem long-term and I started to think negatively about it. That’s the only thing that changed. I’ve had POTS this whole time. I’ve had good days and bad days this whole time. I happened to have a significantly bad period and I’m still in that. The only thing that’s changed is the story I tell myself, and I have to keep catching the story, catching it, catching it.
Now, I know some of you are saying, “No, but my disability is making my life have a lower quality.” I’m not saying that’s just a story. I understand that it’s a situation and a circumstance. So I’m not discounting that. But what we need to do, and this is why I wanted to reflect with you, is to catch the story we tell ourselves about things that are not true, like the future, because we don’t know. We don’t know the future. There may be a POTS drug that comes out and I take it and I’m happy for the rest of my life.
I am going to recognize that having this disorder has had some benefits. It’s forced me to slow down. It’s forced me to be grateful for my medical health, for my legs and my arms, and for my heart and my brain.
This is where I ponder how wonderful that our body tells us what to eat. How wonderful is that? Because when you have POTS, you have nausea. And when you have nausea, nothing feels good to eat. You have to force yourself to eat. Every meal, I have to force myself to eat. Sometimes, I have to tell you guys, I was cracking up. I eat mostly healthy, meaning I ate all varieties. There is no good or bad food. I have a very good relationship with food. I love food. Food brings me incredible amounts of pleasure. I never judged myself for what I eat.
I was telling my sister, who’s a doctor, she was like, “Well, are you eating?” And I was like, “Yeah, I had chicken nuggets for breakfast.” And she was like, “Why?” And I was like, “It’s literally the only thing I could eat. That’s the only thing I could get down. It’s the only thing that sounded good.” And she was like, “Okay, what did you have for lunch?” And I was like, “I had ribs.” And she said, “Kimberley, what is happening?” And I said, “No, this is how it is. I have to...” It’s so hard. And I’m now so grateful for the pleasure around food that I have experienced and hopefully, we’ll experience it again here very soon.
I really want to watch (1) the story I tell myself and (2) the hope catch the hopelessness in its tracks. I know a lot of my patients and I know a lot of you because you’re going through a particularly difficult season like me. You’re telling yourself this season will never end, and it will. Seasons come and go. Some last for longer than others. Sometimes it’s a particularly chilly season, sometimes it’s not. The main piece here is for me to catch the judgment, the stigma.
Here’s another one guys and I hope this resonates. It’s so humiliating. I collapsed right at the entry of the tennis. People were walking past me, and my instinct was to say sorry to every person that passed by. Even though I was pretty much not in consciousness, I was frequently apologizing to my tennis coach, my husband. My tennis coach called my husband. I frequently apologized to him. I apologized to anybody who saw it. “I’m so sorry. I didn’t mean to scare you.” And how much that apologizing was embedded in shame around suffering.
I’m on the floor, completely limp, but I’m apologizing to other people. That is completely related to the shame I noticed that I am carrying around suffering and struggling and not being super, super-duper high functioning. This is dangerous. We have to check this. I’m going to encourage you to check this because the problem with that is it stigmatizes disability in general and it stigmatizes you being a human who suffers, and you will. You’ll have illnesses or struggles like seasons that are difficult. It’s so important that we break down that judgment we have around suffering and disability, meaning when you don’t have the ability to do things. So important.
When we break that down and we work through that, then when we do struggle, there’s not this second layer or fifth layer of pain. It’s just like, “Oh no, I’m just suffering. I’m suffering right now. This is a difficult season.” Instead of, “This is a difficult season. I’m suffering. It’s never going to go away, and I’m weak and dumb and stupid and inconveniencing other people for suffering.”
So, I really want us, hopefully, to learn from my own experience here. Hopefully, this resonates with you where you can really break down the stories and the beliefs and the judgments we have about disabilities. I think it will make a safer place for those who do have a disability. I think it’ll make a safer place for you when you’re suffering. I think it’ll make a safer place for us as a human race around the idea of suffering. It’s so, so important.
The last piece here is when we’re suffering, I noticed this whole back and forth on the solution. Should I do this? Should I go on this medication, that medication, that treatment, these treatments, see that doctor, see this doctor? I’m sure a lot of my patients are like, “Am I doing the right thing? Have I got the right treatment? Have I got the right therapist? Have I got the right medication? What’s happening?” There’s so much indecision around seasons that are filled with suffering.
I just want to validate that. I don’t want to give you advice. I don’t want to guide you in any different direction. I think all I want you to do is to recognize that indecision and not punish yourself by staying there too long. Consult with your doctors. Consult with your therapist. Talk with respected people or people you trust. Be careful of how much mental space indecision takes when you’re in a difficult season because you’re suffering. It’s enough. We don’t need to add. We don’t want to add. We don’t want to make more problems and more suffering for you because you matter and your recovery matters and your healing matters. That’s just something I’m noticing.
It’s funny, every morning, I am negotiating with myself in terms of like, “Will I take my meds today?” I mean, I always take my meds. So I’m not going to ever discard someone from making a medical decision without seeing your doctor. I always do, but I really catch myself going, “Maybe I won’t take it today. This is just too much. It’s too hard. It’s too many side effects. It’s too difficult, too painful, too scary.” And I have to go, “Okay, Kimberley, get your head out of your indecision. Honor what’s right. If you really need to do that, be effective and call your doctor. Don’t spend time in your head.” So, that’s just where I’m at.
What I will say, just in case any of your worries, I am okay. I have a great team. I have tremendous support. My husband, oh my God, he’s just amazing at showing up when things fall apart. He is incredible. I’m so, so lucky. I hope that I don’t worry you with me sharing this.
Someone asked me the other day on social media, “Is it hard for you as a clinician to share this?” And I said to them, “No, really not.” A part of my mission is to de-stigmatize therapy, to take the stigma out of going to therapy. I think a really big part of how to do that is for the therapist to show up as real humans. I think when we do that, when therapists show up as real humans, in the process, we do this stigmatize mental health and therapy because we don’t see the therapist as this person who holds all the secrets and is the knower of all things and is analyzing you instead of just seeing them as humans. You’re just going to therapy to talk to a human who also suffers. I just wanted to share that with you because I think it’s important that I model that to you. That’s one of the things that I hold very strong in my values.
So that’s that. There are my thoughts on struggling and going through a chronic illness and wrapping my head around the stigma of the word “disability” and the concept of disability. So, that’s it. That’s all I have to say.
I hope this has been helpful. I hope that you feel seen and you feel heard. Maybe you have some insight as I spoke. If that’s the case, we’ll then, I’m a happy girl.
All right. Thank you so much for listening. I do know your time is precious, so I’m so grateful to have this time with you. I will continue this conversation as I continue to unpack my own many layers of stuff, of glug around it. I’m very open to continuing to learn. I’m really, really looking and learning around the stigma of disability because it’s something that I have been privileged up until now, not to have to really wrap my head around. So I’ll do the work. I will stumble bravely through this, as I’m sure you are too.
All right. I love you guys. Please go and leave a review. The reviews help other people see this podcast as something of quality. When they see other people’s reviews, they are more likely to click on it, which means I get to help more people, and that is just a blessing. So, thank you. Please do go leave a review.
Please take care of yourself. Please take some time to hold your heart tenderly and nurture whatever suffering you’re going through because you’re not alone and we’re in this together. Okay. All my love to you.
Be on the show
This is Your Anxiety Toolkit - Episode 190.
Welcome back, everybody. Hello, Happy Friday, for those of you who are listening on the release day, and happy day to you who are not.
Okay. Well, how are you? How is everybody doing? I am sitting in my bedroom. We’ve actually had to completely rearrange because our life is changing so much here at the Quinland house. Kids are at school and people are in and out of the house, and it’s very, very different.
So I’m coming to you from my room, and life just continues to change. Have you guys noticed that? It does continue to change. I cannot keep up with it. We embrace. We adapt. We are flexible. We keep trying. We are gentle with ourselves, and that’s the best we can do.
Today, I wanted to talk with you guys about questions.

I have been sort of... What I would say is ‘reflecting,’ but I would actually say, a better word is ‘studying’ the art of asking better questions, and this has been life-changing to me. It has been a practice that I have adopted as per advice of a colleague and a friend in terms of catching the story you tell yourself and asking better questions. Catching the poorly written questions that we now ask ourselves on habit, right? We just habitually ask ourselves not very skilled questions.
Let me explain to you more about this.
When something happens – and you can even do it here together – when something happens in your life, let’s say in the last week or so, something unexpected, unwanted, maybe not so ideal happens, I want you to check in and say, “What is the question I ask?” Some of you may say, it’s a really simple what-if thought question. Like, what if such and such happens? What if ABC happens? What if XYZ happens?
Not a super-skilled question mainly because it’s so open-ended and it’s so in the pursuit of removal of that discomfort. We’ve talked a lot about being uncertain. We’ve talked a lot about willingly allowing discomfort.
Other questions that I have observed my patients asking themselves or reflecting on lately are questions like: What is wrong with me? So they have an uncomfortable, unexpected, not-so-great experience, and their immediate question is: “What’s wrong with me?” And that question never ends. Well, rarely would you have the thought “what’s wrong with me,” and then you respond by going, “Nothing is wrong with me, I am a normal human being responding in the way that any other human being would respond.” We don’t answer those questions. The question sets us up for a failure, just like what-if.
Another one is: “How can I make this go away?” Now, in some cases, this would actually be a really adaptive question. So, let’s say you have an ant invasion in your house. It makes sense. Because we’re highly functioning human beings and we have adapted over time, it makes sense that our question would be: “How can I make this go away?” That in and of itself could be a good question, a solid, skilled question. But when it comes to our emotions, it’s really not. It actually gets us into tons of trouble. Asking ourselves how we can make this go away usually means we’re going to probably have more of it and we’re going into resistance mode.
Another one, which I see a lot of, and I’ve actually done a whole podcast on this one before, which is: “Why is this happening to me? It’s such an innocent question, but yet it gets us into so much trouble because the answer isn’t that great. Why is this happening to me? Nobody knows. It’s not the answer we are looking for. Or the answer you probably catch giving yourself is, it’s because there’s something wrong with you. Go back to the first question because you did it wrong or because you shouldn’t have, or because you’re bad, or because you’re weak, or because... The list goes on and on and on. It’s rare that you’ll go, “Why is this uncomfortable thing happening? Oh, because uncomfortable things happen sometimes.” Again, none of these are bad questions. They’re just not super effective.
Another one, and this is the last one I’ll use as an example, is: “What does this mean?” Oh, that’s a really bad one. It can get us into so much trouble. “What does this mean?” And before you know it, you’re 20 minutes in going around and around, trying to give meaning to something, which probably has no meaning at all.
The reason I really want you to first reflect on what questions are you asking yourself is you’ll probably find that the questions you’re asking yourself are setting you up for self-criticism, self-doubt, punishment, a lot of negativity, maybe for some really unhelpful emotions, and we want to get better at asking better questions. We want to be skilled at asking skilled questions. The questions we ask ourselves can then move us to and into an action that helps us and is beneficial and effective and kind and less work. Less work is good. We don’t want questions that, again, can give you more work. Go back to “How can I make this go away?” Oh my goodness. That’s a lot of work.
Okay. Let me give you some questions that I am practicing when uncomfortable things happen, events, experiences, emotions, and so forth.
Okay, first question. What emotion right now am I not willing to feel? So, let’s say somebody you love has judged you. Okay, that’s not going to feel good. Your instinct is to make it go away. But we’re going to say, “What emotion am I not willing to feel here? Oh, it’s embarrassing. It’s vulnerability. It’s sadness.” Okay. That’s the emotion. At least now we know, we know what it is.
Again, what emotion am I not willing to feel? Let’s say you did an exposure and you tried so hard and it fell apart and you had a big panic attack and you couldn’t back out. Okay. Your question would be: What emotion am I not willing to feel? Maybe it’s fear. “Oh, I totally backed out because I didn’t want to feel fear. I didn’t want to feel uncertainty. I didn’t want to feel doubt. I didn’t want to feel dread, impending doom.”
Next question: Is it true? Let’s say you... This was me the other day. I’m unpacking the groceries and I’m so happy because we picked them up and we didn’t have to go into the grocery store. I just love this. It’s one of the silver linings of COVID – the grocery stores are so good at doing drop-offs. I bring in this huge bag of groceries, and off the counter I fell a spaghetti sauce bottle and glass and spaghetti sauce is everywhere. Your original thought again is like, “What’s wrong with me?” And then my next question is, “Uh-oh,” instead, “is it true?” The thought I had is like, “You’re so stupid. Why are you going to be so clumsy? Is that true?”
Now, I’m not asking that question to invite a long layer of rumination. In dialectical behavioral therapy, it’s called checking the facts. When you say a negative thing to yourself, check the facts. If I said that in a court of law, what would the jury decide on? “Kimberley is an idiot. She should have known better.” I’m pretty sure the jury would say, “There’s no way Kimberley would have known the specific weight of that jar, and the edge was so close and that it was going to fall at this angle. We’re actually going to probably let her off.” Is it true? Check the facts.
Now, a quick note there. If you’re having OCD obsessions, we don’t need to check the facts of those because that could become compulsive. I’m talking more here about things we say to ourselves like, “You are bad. You are dumb. You are stupid, what’s wrong with you?” Those kinds of comments and more depressive thoughts like, “The world is bad. My future is going to suck.” You may want to ask yourself, is it true?
Now, if your instinct is to say, “Yeah, it’s true. My past has been crappy. So, therefore, my future will be too,” I’m going to say, “I don’t know if that’s going to stand up in a court of law. Because they did it once does not hold you guilty. If it’s happened a hundred times, it still doesn’t give me enough evidence to convict that your future is going to be bad.” So let’s just stop and check in with what we’re saying.
Another question. This is my favorite, guys. This is the king of all questions. I really want you to get good at asking this one – what in this situation would the non-anxious Kimberley deal? What does the non-anxious you do in this situation or with this emotion? Best question ever. That’s a really solid question right there. It doesn’t mean you have to do it all perfectly, but it at least let you inquire as to how you would act, given that fear wasn’t there to make your decisions. How would your values have you act? How would your character have you act in this situation?
So, if I, let’s say, was going to take a test and my fear was saying like, “What if you fail? What’s wrong with you? You should be better than this. You should be fully prepared. You’re asking not-so-great questions,” and you said, “Okay, what would the non-anxious Kimberley do right now?” It would be: “Okay. She would get a drink and get a piece of fruit and eat it and then go and take the test. She would be kind and she wouldn’t be ruminating about how it’s going to go bad.” Okay, go do that. That’s your blueprint on how you should be acting. That’s the skills and the perfect outline of what direction you might want to go into. Fabulous.
And the last question... You can have more, you can add more to this. I want you to really think about it because I want this to be specific to you. But the last question I want you to ask, the question I think is a really good question, which is: What do I need? Not what do I want, but what do I need? What will help me here? What will help me get my long-term benefit here? Get me to long-term recovery? What do I need?
Let’s use a couple of examples. You’ve just spilled spaghetti sauce all over the fridge and the counters and everywhere and there’s glass everywhere. What do I need? I need to be kind to myself. I need to take my time cleaning this up because my instinct was to clean it up in a rush because I was like, “Oh, this shouldn’t have happened. What’s wrong with me? I’m going to clean it up in a real rush so that I can get to my happy things.” But the problem with that is, it only ended up making me more aggravated because I was rushing. So what do I need? I want to clean it up gently and slowly, compassionately.
Let’s say you’ve just done an exposure and it didn’t go so well and you had a massive panic attack. What do I need? I need to slow down. I need to celebrate my attempt. I need to breathe. I need to reflect on how that went and what got in the way. I need a nap. Sometimes when we do exposures, we need big naps, and that’s fine. What do I need?
Someone just said something really unkind to you. What do I need? I need to cry. I need to feel my feelings. I need to give myself permission to be sad. I need to call a friend. I need to maybe set a boundary with that friend. Much better than saying, “Why is this happening? What’s wrong with me? how can I make it go away? What does all this mean?”
So what I want you to do is I want you to leave today’s episode and I want you to spend the day or the week or the month thinking about what are good questions, how can I ask myself really good questions, better questions? Be really intentional about this.
I often say to my patients, if your thoughts are a dog and you’re the owner of the dog, sometimes we let our thoughts just go all over the shop. We just let them go. We follow them. If the dog is sniffing into one corner, you go with it and you sniff into one corner. Sometimes with our thoughts, not so much the intrusive thoughts, but the thoughts we say about ourselves, the criticisms, the stories we tell ourselves, sometimes we’re going to yank on that chain a little bit, on its leash, and be like, “Come on. No, no, no.” We’re not going over into that corner and sniffing out that horrible hole. No, we’re not doing that today. We’re asking better questions.
You’re allowed to do that. That’s not thought suppression. That’s being skilled with your cognitions. We’re not trying to prevent thoughts. We’re just catching when you’re spiraling on them and you’re yanking on the chain. And then come on back. You’re going too far. You’re resisting too much. Let’s lean in.
I hope that’s helpful. Ask better questions.
Thank you so much for listening. I am going to ask you for a favor. Would you please leave us a review? It would help us so much, us meaning all the team at CBT School. We are working really hard to expand our reach to help more people, provide free content. So if you would be willing, I would love nothing more than for you to leave an honest review on Apple podcasts or wherever you listen. We are going to give away a free pair of Beats headphones once we hit a thousand reviews. So I’d love for you to be in the running for that. Thank you.
All right. I love you guys so much. I hope you’re doing well. I’m thinking of you always. I’m so grateful I get to spend this time. Thank you. I know your time is valuable.
Have a wonderful day. It is a beautiful day to ask better questions and do hard things. Let’s do it.
Have a wonderful day, everyone.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Hello friends, you are going to love this episode. Holy smokes, I just recorded it, so you’ve got me fresh, and I’m so excited. I just had such an amazing conversation with Mike Heady. He is an LCPC and he treats OCD and anxiety disorders. We talked about shame and shame and shame and shame, and he brought so much wisdom. You guys are going to love this episode. It is packed full of all the good stuff. So, I’m not going to waste your time. I just want you to get straight there and listen to it.
Before we get started, if you haven’t left a review, please do so. I love getting reviews from you. When we get good reviews, it doesn’t just stroke my ego. That’s not the point. It is because the more reviews we get, the more people will come and listen to the podcast, which means then I get to help people with these incredible tools, these science-based tools. Hopefully, even just from today, if you’re first time listening, welcome. We are talking about shame, and you are going to get so much from this. So if you are listening, please do leave a review. I would be so grateful. And enjoy the show.
-----
Kimberley: Welcome. I am so excited to have with us today, Mike Heady. He is an LCPC. That’s correct. Right?
Michael: That is, yes.
Kimberley: Yes. We’re going to have a conversation that actually might be my favorite topic in the whole of the podcast. We’re talking about shame. So, welcome.
Michael: Thanks for having me. I share your passion for the conversation.
Kimberley: Yes. Not that I love shame, but I like talking about shame.
Michael: Yes. I agree. It’s hard to say you love shame. It’s like saying I love fear.
Kimberley: Exactly. So, why are you interested in this topic?
Michael: It’s been a professional evolution for me, originally being trained to treat anxiety disorders and OCD. We talk a lot about fear and uncertainty and we have a ceremonial way of responding to shame. We’re like, “Oh yeah, and there’s a shame too.”
In the last couple of years, I’ve really done a deep dive into like, “Well, what is this?” Because a lot of clients are having a hard time getting better. I don’t think it’s the fear that’s hard for them to get past sometimes. I don’t think it’s the uncertainty. I think it’s the shame. I think it’s a different animal. When I started doing a lot of digging, I realized there’s a whole world of shame out there in the literature, and how it applies to OCD fascinated me. So, that’s my new passion project.
Kimberley: Yeah. Same. Exact same experience. Also seeing how much fear in and of itself is a generator of suffering. But as you said, there’s this shame that’s generating suffering at exponential levels. So, I’m so grateful to have this conversation with you. for those who are listening and who might not really understand shame, would you be interested in giving me your working definition of what shame is?
Michael: Sure. Are you okay if I elaborate on it a little bit?
Kimberley: Yeah. Go for it.
Michael: Okay. I think a good definition is that shame is a really painful, aversive, unpleasant emotional experience. Fear or disgust, it’s natural or instinctive for us to want to back away and get rid of shame. Shame is often brought on by some kind of real or perceived violation of a social norm that we actually believe in. So it’s not this mystical emotional thing. It’s a thing either real or perceived occurred. And then I experienced this negative, painful emotion of shame. That’s the short version of the definition.
I think it’s worth talking about shame as having two levels of shame. We might call an adaptive kind of shame, the shame where we view it as a response to a specific episode, rather than some generalizable character flaw or full-on assault of our identity. I violated something I believed in, I feel bad, which is different than guilt because guilt is about apologizing to the other person for something you’ve done. But I might feel bad for violating a norm I believe in. Okay, there’s nothing toxic about that.
There’s another level of shame that we tend to want to talk about more. It’s the toxic shame. That’s the shame that is unworkable. It’s always unhelpful. It is a response to a perceived or real violation of a norm that has broad sweeping characteristics to it. It is a full-on assault on our identity. It is a condemnation of the self. That’s the toxic shame.
I can wrap up this as saying, what was incredibly helpful for me when I was going deep dive into what shame was is, yes, shame is an emotion. We know what emotions are. We all feel emotions. We’ve all felt shame.
You and I, as therapists, spend our careers trying to help our clients have a different relationship towards painful emotions, and understanding what an emotion is, specifically around shame, I think was really enlightening for me. I derive a lot of this understanding from some work that occurred in the sixties and seventies, probably before then, but the work from the sixties and seventies is what brought it to my attention, that emotions are an emergent experience constructed by an interaction between our biology and our biography.
The biography piece comes out of Silvan Tomkins work in the late sixties where he suggested that, yes, there’s a universal kind of biological experience that contributes to an emotion. But the part that completes it is our own narrative, which is unique to us.
My interaction with the world, as I develop from a child to an adult, the experiences I have, my environment, that’s the secret ingredient to my shame. So what makes me feel shame isn’t necessarily what makes you feel shame.
For instance, if I were to, while talking to you, suddenly break out into a red flush on my face, start sweating, and my voice start cracking, I might experience that as an embarrassment, like a small shame. But if you perhaps had terrible social anxiety disorder and the same thing happened to you, the same exact event, you might see that as a humiliation. Both are derivative emotions of shame. But humiliation is different from embarrassment in orders of magnitude of pain. Humiliation is closer to trauma than it is to anxiety. This is anyway my long-winded way of saying, yes, shame is a complex animal, and that’s the working definition I tend to have.
Kimberley: Yeah. It’s a different way of explaining it. This opportunity makes me so happy. What you’re saying is, it’s on a spectrum, would you say?
Michael: Oh, absolutely. Yeah.
Kimberley: Now, let’s play that out. We’re talking about the biology, and then there’s the story we tell ourselves. Would you give an example for you? You and me, let’s say we both got embarrassed. Let’s say we both made a mistake or something. We embarrassed ourselves in front of each other, which is not going to happen here. But if we did, what might be a difference in the story we told each other which would indicate that higher level of shame or toxic shame?
Michael: Sure. Let me clarify the story. It’s not just how we appraise the shame itself. That’s a part of it. But the story is like my upbringing. I was brought up in a blue-collar family. There wasn’t a lot of room for emotions, especially for the male members of the family. So if I encountered a situation where I felt vulnerable or sensitive or hurt, the expression of that emotion could be shut down. That expression of that emotion could be punished, ridiculed. Not that I was ridiculed, but it could have been.
Someone’s narrative about a negative emotional experience could have been that and ongoing. They could have been bullied for being a sensitive kid, whereas you may not have. now you both may experience the same thing as a generic sense of shame. “I wasn’t the way I wanted to be. I wanted to be put together and intelligent and I made a stupid GAF, and I came across looking silly.” One kind of embarrassment for one is not necessarily the embarrassment for the other. That’s what I mean when I say “the narrative.”
Kimberley: Yeah. Okay. This is wonderful. I think that maybe we want to take a look at, and I know I have a few questions. What I’d love to take a look at is, why would, let’s say someone feel shame for having a mental illness?
Michael: Well, yeah, that’s a great question. I think there’s a whole lot of reasons why someone might feel shame. One of them could be, I feel shame because the mental illness – we can say OCD in particular since this is one of the things I primarily treat – is that the content of my obsessions themselves could have a taboo theme or they could be otherwise conceived as bizarre. That’s going to create a sense of “I shouldn’t have this thought, there’s something wrong with me I have this thought.”
The helping field, in general, commonly misinterprets and doesn’t understand OCD. If you present this set of thoughts to them, you’re going to get a sense of judgment and rejection or humiliation, and that’s not made up fear. That’s a real fear. That stuff happens to people. That’s an example of how someone with a mental health issue can develop shame. It’s because they may have gotten that feedback or fear rightfully so that they would get that feedback.
Another way of looking at it is just, “I shouldn’t have this because having this means I’m not working properly. I’m otherwise defective or broken.” It’s a silent problem for people – these emotional and psychological things. We have a lot more empathy and understanding for people with a physical problem than we do for someone who has a psychological or emotional problem. So, I think that there’s this built-in--
Kimberley: Stigma.
Michael: Yes. Stigma. Right. Thanks. Yeah, exactly. And then there’s the people who’ve tried to get better. I’ve certainly seen a number of clients who’ve gone through years of therapy. They’ve worked diligently with great therapists, all very well-intentioned, and they failed to get better. “What’s wrong with me? I must be really broken.” I’m sure there’s countless other ways, but I’ll pass that off to you, I think.
Kimberley: Yeah. I mean, I think these are all societal expectations that are placed on us. It’s funny, you brought up the question about the concept around being humiliated for having an emotion. Somebody had written a question like: How can I be considered “the man of the house” if I have anxiety? I mean, there’s so much shame in that question. There’s so much societal expectations in that question and stigma in that question.
I think it’s definitely there, and I think you’re right. For the things that are unknown, I see that to be more shame. I think everybody understands sadness. So we don’t feel so much shame around it. But fear of harming your baby – let’s not talk about that. You know what I mean? Let’s push that down.
Michael: Right. And not only because it’s universally taboo. We know that instinctually. We don’t need to really be told that. We know that, because that’s our response if we were to hear that from someone else. Until we have that intrusive thought ourselves and they’re like, “Oh, me too?”
Shame, I think it’s distinguishing shame from the other negative emotions that people have, because I don’t think they’re all the same. Oh, negative emotions or negative emotions – let’s just learn how to handle them. Fear, that’s a tough one. But shame? Shame is the most painful.
Kimberley: It’s ouch because it’s in silence too, I think. My thing I say all the time is that shame thrives in secrecy. One of the best things you could do is to tell it out loud.
Michael: I was having a conversation with colleagues about this a couple of weeks ago, and someone brought up a slogan that comes from AA, which is, “We’re only as sick as our secrets.” It’s such a powerful message. The idea that speaking that secret allowed, speaking that shame aloud can be healing. Now it can also be traumatizing. We can probably get into that later in the episode. But I think that there’s discernment about how and who we share with, and us as therapists creating a space where that’s good and healthy for the person. But you’re right. Absolutely. The things that thrive in darkness are painful.
Kimberley: Okay, so you have a client and they have just very typical symptoms of OCD, even if it’s very typical taboo, obsessions – this is for people listening – any disorder, depression, BFRB, eating disorders, how do you work with that shame with your patients?
Michael: That’s a fantastic question. I’m always evolving on how I figure that out with a particular client. I think if I were to try to distill that down to something helpful to the listeners, I think as a therapist, it would start with the very first interaction I had with the client. The first contact is the first opportunity, probably the best opportunity to provide a safe space that’s understanding, validating, authentic so that the client can then experience this interpersonal interaction that they’re having with this therapist as welcoming towards disclosure of a secret or their shame.
I think that that first contact is vital. You can come across as the kind of person they want to talk to and try to set the stage and make that an effort, build that therapeutic alliance, continue to work on a therapeutic alliance because if you don’t, it might be a lot harder to build the work to let them disclose that shame.
And then from there, I think education about what shame is, like I brought up in the beginning, that shame can exist on this continuum, that there is actually an adaptive kind of shame. We don’t tend to talk about it. We don’t tend to see it because we talk about the toxic and the pathological shame, the one that keeps people stuck in hurt. Through that education, through a demystifying of it, I think, is incredibly valuable.
I’ll talk about the compass of shame in a minute. I don’t want to steal all the time from you. It’s like I talk a lot.
Kimberley: Go for it. No, do.
Michael: I’ve been thinking about this in preparation for our conversation today. I was thinking like, how would I want to set up an ideal way of dealing with shame with a client and again, creating that therapeutic space that they’d want to share that. And then if we have this experience that once we hand our secret or shame over to another person like, “Here you go,” that’s what the clients are doing to us, they’re handing it to us.
If we receive it and hold it with compassion and understanding, if we hold it with acceptance of them as a person, I think we introduced them to common humanity – one of the three things that show up with self-compassion, that common humanity – perhaps for the very first time in their life. Because this is such a secret, quiet problem, this might be the first time they’ve ever been met with common humanity and acceptance when they’ve revealed this. I think that’s immeasurably powerful for the client. I think it helps them create a healthy distance from that narrative that’s been telling them to keep it a secret, keep it a secret, or else you’ll get rejected. “Wait a minute. I wasn’t rejected.”
Kimberley: Yeah. It normalizes it too. Right?
Michael: Yeah.
Kimberley: Sometimes when I hand over the why box that has all the different obsessions, that in of itself can be a shame killer because they’re like, “Oh my goodness, all of the things I have are right here on this piece of paper and you don’t seem alarmed at all.”
Michael: Yeah. I’ve had email interactions with clients who are like, “Have you ever heard of this kind of presentation?” I’ll shoot them links to three books written about it. They’ve written entire books about this so you’re not alone. It’s so helpful for them.
Kimberley: Yeah. Tell me about the compass.
Michael: Yes. I was introduced to this through one of my mentors, and it really rang true for me as a useful concept. The compass of shame was developed in the 1980s by a psychiatrist by the name of Donald Nathanson. I don’t want to bore the audience with the history, but he researched shame basically that was his career. Nathanson had found through his research that there are four predictable and common unhelpful responses to shame. I’ll say toxic shame. We’re all talking about toxic shame. Those four represented the four points of a compass – north, south, east, and west. It doesn’t matter where they go.
One of the points is withdrawal. Withdrawal is when we get quiet, silent, small. Like a dog who got caught chewing on the cash knows they did wrong. They get small, they get quiet. They try to disappear into the moment. That’s one common response to shame.
Another one is avoidance, behavioral avoidance of situations and people and circumstances, but also through substances, through food, through sex, through anything that would be a direct response to a cue, “I’m going to avoid this feeling.”
Then another part of it is to attack others. This shows up when you felt humiliated or embarrassed by someone else. Someone made you feel this way, so you’re going to lash out verbally or physically. In a sense, the way I think of it is in the sense of trying to balance the scales. “You’ve made me feel small and vulnerable and insignificant. I’m going to try to balance that out by making you feel the same way.”
The last one I think by far the most common in the people that we’re going to be working with is attack the self. This is self-criticism, this is berating ourselves, self-condemnation, degrading ourselves. It’s often seen as “I’m going to be holding myself accountable for this failure real or perceived,” and that’s going to make it better, that there’s somehow a utility to this attacking self-response. But when you poke at it just a little bit, it’s completely unhelpful. It’s just a massive perpetuator of the problem.
So, that’s Nathanson’s Compass of Shame. I think his point in bringing this up is, look, everyone’s toxic shame response is going to fall probably into one of those four. Where do yours? if we can bring awareness to that, maybe we can learn to pivot to a more functional or helpful response instead.
Kimberley: Right. I think that that awareness, again, it’s validating and it’s normalizing the normal response to shame, which helps the shame, I think, in and of itself. Okay, so let’s play this out. If something happens, you’ve made a mistake or you’ve had a thought that you’ve deemed unacceptable, or you showed up in a way that created shame, you did all four of those things, what do we do from there? Or you did one of them. Now that we have this awareness, how might we meet shame instead in your thoughts, in your mind?
Michael: I think hearing that from a client and I was watching it unfold in the moment, I might say, “Can we pause for just a minute? I think shame showed up for us.” He might even be able to see some of the behavioral changes in their eye contact and the postures. I think shame showed up. What are you doing with that right now? Because again, it’s silent. It’s not broadcasting this out loud. It’s silent. What are you doing? What’s going on in your mind?
Probably reveal what you said, they did one or all four of those things – I would point that out, give it a name. We understand this process. This is somewhat of a predictable response. Can we hit the pause button and can we now make a choice to pivot to a different response. Pivot to what? Pivot to self-compassion maybe. That might be a teachable moment. What is self-compassion? Can I give you an experiential exercise on meeting this moment with self-compassion? I can model meeting this moment with you with compassion so you can see what that looks like and feels like.
Instead of spending time in the head, in the verbal, in the ruminative come back to the feeling, because that’s what we’re trying to avoid. When we criticize ourselves, we’re trying to avoid and escape criticism, or using criticism to try to avoid and escape shame and humiliation. Okay, let’s come back to that. That’s painful. We can learn how to sit with that without having to beat ourselves up or escape it.
I think people can sit with it in different ways. You can use it as an exposure opportunity for people who are feeling smaller kinds of shame, like embarrassment, like let’s do some exposure towards what it feels like to be embarrassed. If we’re dealing with a much more painful kind of shame, that humiliation kind of shame, let’s meet that with more direct self-compassion in this moment.
I think it gets sticky a little bit when we introduce self-compassion, if we haven’t already introduced it, because like any intervention, it hinges on the client buying into it and thinking that they deserve to receive it.
Kimberley: Right. I’ll give you my personal experience with this because I think, and I see a lot and I would add a fourth point to the compass, which is, now as you’re talking, I think this even different than what we talked about in previous conversations, just the two of us, is I think if I were really to track it, I think that another thing that I did when shame showed up is I swing into perfectionism. The stronger shame was, the more I would do good or be good. It’s an interesting reflection for me because I think the more I felt imperfect and the more shame that brought up, the more it’s like compulsive do good kind of thing, which I think again, might be why some of our clients get stuck around shame because there is that sort of self-punishment. “Well, I did a bad thing. Well, I have to neutralize that with a positive, good thing.” I don’t know. Just something I’m thinking about.
Michael: No, I think that’s really great. I’m sure a lot of people listening are thinking right now, nodding their heads, “Yup, I go into perfectionism.” If I can channel Nathanson for a second, I imagine he would say, “That’s a type of avoidance. It’s an avoidant behavior. You’re doing this thing and it’s a compensation to numb, or to balance the scale.” If I do enough good, it cancels out the bad. The message is that that thing is intolerable to feel, and it’s not.
Kimberley: Good catch. That’s true. It is. It’s like neutralizing the compulsion, right? Yeah. Okay. This is amazing. I have some questions from the audience that I think is a perfect segue, and there’s one that really hit me, really deepened my heart and I wanted to ask your opinion on. Somebody had asked, how do I manage shame for having symptoms? They didn’t express which ones, but I’m assuming it’s having symptoms of being a human of some respect. But I also have privilege and resources and the ability to get care, how do I manage shame when I have privilege?
Michael: That’s a really great question. I think if I can flip that around a little bit, I can say that the cost of your privilege towards access to care, towards a good community of people, the cost of that isn’t more shame. We don’t want to shame ourselves for having opportunities. In a way, it moves you away from doing something about that, about that privilege. If you recognize I have privileged shaming yourself is useless. Who’s that for? That’s a silent response to try to balance out this. It’s an avoidance. It’s a running away from.
So can we try to meet that? I’d say first with patients and then recognition, yeah, there is some privilege here and I feel bad about that, and then move into a “what’s next” kind of a mindset. Like, I still need to work on my own shame about having these symptoms. It’s not like I have to suddenly stop working on that because I also happen to have the privilege and the capacity to work on those.
But I think we throw it into the same mix. It’s like, okay, so you’re shaming yourself. Which one of the four points of the compass are you doing now in recognition of a privilege? Once we get off of that unhelpful response, we can then maybe find a more helpful way to recognize the privilege, to speak out against the privilege, to prop other people up and help other people have access, things like that. But we can’t do that if we’re shaming ourselves, because shaming yourself, criticizing yourself, avoiding isn’t workable.
Kimberley: Yeah. There’s so much of this like self-punishment involved as a response to shame. Like, okay, so I have this one privilege, so I must be punished for that before I can address the problem that I have almost. I’m so grateful that you answered that because I have seen that multiple times, many, many times with my patients and I’m guessing you too.
You’ve talked about shame around lots of emotions. Interestingly, there were two very common questions, and I’ll leave these as the last two questions for you. There was a lot of questions around having shame for anger and there was a lot of questions around having shame for having a “groinal response,” which I’m assuming is in relation to some kind of sexual obsession or maybe even sexual orientation as well. Can you share your thoughts on those?
Michael: Sure. Shame around anger, I think... I’m trying to interpret the question a little bit. I imagine it goes beyond just the feeling of being angry, but maybe the act of being aggressive, if I can make some interpretation there. I helped the client recognize that anger, like any other emotion, is universal. It’s an emergent experience. It’s not really up to you about whether you get angry or not. We don’t have to act on the anger. We don’t have to become aggressive either passively or physically aggressive about it. So, teaching them that there is some workability in our response to anger and that if we accept anger as an emotion, if we make room for anger as an emotion, we don’t need to have a response to it in the same kind of way. We can let it in.
Susan David, in one of her Ted Talks, she said that emotions are data, not directives. I love it. Super helpful way of organizing your thoughts around that. It’s just, let the emotion be data. It’s if you’re responding to something in your life, something happened that it shouldn’t have happened and it wasn’t fair, and then you felt angry. Okay, I understand that process. I don’t need to do something about it to get rid of it because there’s that relationship to an emotion that can be unhelpful. Now I have to find a way to control or get rid of it. Notice we only do that with the negative side of emotions. We don’t tend to be like, “I have to get rid of my joy.”
Kimberley: Too much joy.
Michael: Too much joy.
Kimberley: Unless we feel privileged, so then we’re not allowed to have too much joy.
Michael: Right. Yeah. In response to the groinal stuff, I think, again, it comes down to your biological, your physiological, your groinal response isn’t really up to you. I think Emily Nagoski does a really great job in her talk about unwanted arousal, and such a powerful Ted Talk and really great education around that. Your body’s going to respond, whether you like it to or not. I used to joke around and say, the reason why the 13-year-old boy isn’t standing up at the end of Spanish class is because he wants to get more lessons. It’s because he’s waiting to not be embarrassed when he stands up. It’s not that he’s attracted to Spanish as a language –maybe he is – it’s because he had a response and it wasn’t really up to him.
Okay, so bodies respond to things. Can we separate that out from the thing that was in our mind? Bodies respond to sex generically. It doesn’t matter who it’s with, what it is. Just the idea of it, the notion of it, the hint, and it response. So even people listening to us now, using the words like sex, might respond to the word, and that doesn’t mean you’re attracted to the word or to this podcast. Maybe you are, but it’s probably not. It’s that your body responded to things because of all these associative learning cues that are going on. That education is powerful.
And then, of course, I treat shame the way I treat any toxic shame, which is, the response to it is the biggest problem that needs to try to meet it with something a little bit more akin to self-compassion and common humanity.
Kimberley: I love it. Thank you. Oh, you nailed it. Is there anything else you want to share?
Michael: I mean, not off the top of my head. I’m sure that we could dive into so many different rabbit holes on the subject, but I think this was a good intro to it.
Kimberley: Yeah. Intro, but also with depth. I’m really grateful. I love to give as many applicable tools as we can. I feel like there is some better understanding. The compass is so good. It’s so helpful to be able to deconstruct it that way.
Michael: Yeah. That was a game-changer for me when I heard about that too. I will add a couple of things, just in passing other ways of therapeutically addressing shame. Once we’ve agreed that those four points in the compass are not the way we want to handle it, we have to have a new way. There’s a, what used to be, I think, a Broadway show called Get Mortified. It’s now a podcast, and it’s people sharing humiliating and mortifying personal stories. Again, this is going out to strangers and this is an idea that I’m normalizing these experiences in my life. Maybe someone else can relate to it and maybe we can bring some humor to it. It’s not about making fun of the person or the situation, it’s about saying, can we all just laugh at the fact that we’re busy concealing something that is so universal and ubiquitous.
Kimberley: Yup. Life happens, right? It doesn’t go to plan.
Michael: Yeah. I think that’s the other piece. Once you’re ready for it, humor is hard to think of a more helpful response to shame.
Kimberley: I’m holding back every urge right now to be like, “What’s the most mortifying thing that’s ever happened to you?”
Michael: That’s a different podcast.
Kimberley: I was once on a podcast where he asked that, a very similar question. It was on OCD and he asked me a similar question. I think I completely went into your shame compass, like all the things, “What can I do to avoid this conversation?”
Michael: Yes, yes. I think that would be like a few cocktails and we’re going to record a podcast and maybe we can talk about that. But again, you can see, you can notice how even here, I could easily come up with two very shaming experiences in my life, and the difficulty of sharing that when I think that other people are listening to it. Why should I care? It’s because it’s a painful emotion. So even us therapists have a lot of work to do with personally so that we can show up with the client in a way that’s helpful.
Kimberley: Right. When I was doing one of the Mindful Self-compassion intensives, this is with Kristin Neff and Christopher Germer, one of the activities where we had to stop and do activity with the puzzle we came with if you came with someone. And then you had to turn to a person you didn’t know, and you had to tell them one of the most painful things that’s ever happened to you. They didn’t really give you a lot of choices either. They were like, you’re here, you’re going to do it.
The whole act was there was tears everywhere, flying across the room. But the thing was then, the person who’s listening was not allowed to say anything, except “Thank you for sharing.” It was so powerful. It was so powerful. They weren’t allowed to say, oh. You weren’t allowed to touch them. You weren’t allowed to say anything, except “Thank you for sharing.”
Michael: And again, an immeasurably effective and important thing. That wasn’t self-compassion. That was compassion, right? This is why I think like you with your Instagram work and people like Chrissie Hodges and OCD peers, and anyone who’s an advocate for OCD that is building a community of people where they can interact like OCD has a community of people. These communities allow other people who are struggling with OCD to interact with each other. You create this group acceptance. The group has accepted you in, shame and all. You no longer need to conceal or keep secret this thing. The weight, the anvil that gets lifted off your shoulders, you no longer have to be weighted in the past.
It’d be nice if we could generalize that outside of an OCD community and just say, the community at large has now been sufficiently educated about what OCD is and isn’t, what depression is and isn’t, what eating disorders are and are not, trauma, so we can be a lot more understanding of one another. Perhaps that’s a little Pollyanna-ish to hope for, but I think that that’s the direction we should head on.
Kimberley: That’s the mission. Yeah. Well, I actually think that this is a perfect place for us to end because I think that that is where we’re at. That common humanity, we all have it. You’re not alone. Yes, it’s the most painful thing you’ll feel. You’ll feel like your heart is breaking at the time. All of these things are so normal and part of being a human. So I love that that’s where we’re at. Thank you.
Michael: Thank you for indulging the conversation.
Kimberley: Easily, so easily. Tell us about where people can hear more about you and know about you.
Michael: Sure. As you mentioned, my name is Mike Heady. I’m the Co-Director of the Anxiety and Stress Disorders Institute of Maryland. I work with my other Co-Director, Dr. Sarah Crawley, who’s a Child and Adolescent Psychologist. The Executive Director and Founder is Dr. Sally Winston. She’s written a number of books on OCD. We’re in Baltimore, Maryland. We’re an outpatient, private group practice. We have over 20 clinicians that specialize in depression, OCD, anxiety disorders, and other related conditions. Yeah, that’s us. That’s me.
Kimberley: Amazing. Well, thank you. I really am grateful. I feel so calm after these conversations too because I feel like it’s the more you guess, you get to settle into it. So thank you. I’m so grateful personally, and for the community here, who sounded like they were very excited about this episode.
Michael: Well, thank you for having me on.
Kimberley: My pleasure.
-----
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
 Welcome back, everybody. Thank you so much for joining me. I know your time is very valuable and precious, so thank you for spending your time with me.
Welcome back, everybody. Thank you so much for joining me. I know your time is very valuable and precious, so thank you for spending your time with me.
Oh goodness, I have so much to reflect on with you today. I’ve had a few aha moments, which I wanted to share with you because I wondered if I’m having these aha moments, maybe you are too.
Let’s just actually get straight to it. Shall we? Because it’s funny for me to say this to you. I’m sort of embarrassed to say this, but I also think it’s very hilarious.
I consider myself to be a very mindful person. I really do. When I’m struggling, I always practice what I preach. I observe that I’m struggling. I bring my attention back to the present. I engage back into the present and I usually feel better. This has been a profound practice for me in my life. I teach it to you guys because of how much of a huge difference it has made to me.
What has been really interesting is, I have taken some time off. I’m slowing down with work. My children have gone back to school. To adjust, we’ve had some massive, massive adjustments in our family. My husband took a year off work to be with the kids, so he could be their teacher. I, when COVID hit, went deep into just so much work and was really working to support the family in a way that I hadn’t had to do before. I’m so grateful and I really recognize how privileged we were to have this environment and this experience because I was writing a book and I had my clients and there’s just no way he could have gone to work.
So, he’s gone back to work. My children have gone back to school. I’m still finishing up the final stages of the book. So, it’s been such a huge difference for me. Because of this, I actually have been working with a coach, which usually I go to therapy every week. My therapist and I agreed that I would take some time off because I really felt like I was doing everything that she had given me. I was really feeling like my mindfulness skills are really helping me.
What was so interesting was that my coach – and this is not a coach for anxiety, this is more of a life coach – brought to my attention – and this is where it’s really funny – that even though my mindfulness skills are really effective and so healing and wonderful, he felt – and I thought it was shocking to start with, but I think he’s right– that I’m using it to avoid feeling my feelings and avoid feeling the sensations of anxiety.
Now, when he told me this, I’m not going to lie, I wanted to smack him upside the face. I was just really mad about it. I was like, “What? You’re telling me, I’m just this girl of mindfulness?” I don’t really see myself as a girl, but my ego was like, “I’m a guru at this. I’m so good at this. You’re telling me that it’s not effective?” I took some time. I shook off the pride, the pride issues that I was having, and I really let what he was saying to sink in. He’s 100%, right.
I really am so grateful for this opportunity to be called out on this one. So here I am sharing with you that I too am going through a layered experience of recovery. As many of you know, I’ve had an eating disorder, I’ve had anxiety my whole life. I have struggled with depression. I have struggled with medical issues that have been really, really stressful on myself and my family. I have handled them mostly really well, I think, but it never occurred to me in this idea of recovery that I may be bypassing the opportunity to really do some work around uncomfortable feelings and uncomfortable sensations.
Here I am. I’m going to teach you what I’m practicing.
Now, I’ve made some adjustments. Instead of noticing my discomfort and suffering, I tend to it with mindfulness and self-compassion. But instead of jumping straight into those skills, which are so good, by the way, I’m not discounting. These skills are gold. If you have mindfulness skills, it’s better than gold. It’s more valuable than gold or anything else that you could get. So I still am going to use those, but there’s this teeny tiny little space before that where I’m actually practicing feeling, allowing, and tolerating uncomfortable sensations, allowing uncomfortable feelings to be there.
Now, I know the title of this episode is How to Tolerate Uncomfortable Sensations. The reason I’ve done that is because even though I realized emotions was the thing I was avoiding, really when I get down to it and we break down a feeling, a feeling is just a combination of a thought with a sensation.
I’ve done episodes on how to tolerate thoughts, but I really wanted to really practice, and this is what I’m doing: Okay, I’m feeling sad. I’ve had a lot of sadness lately show up in my body. Where does it show up? For me, it’s right at the front of my shoulders. I want to just pull my shoulders forward and curl my spine into a C-shape and just contract and go into fetal position. When I feel sad, I just want to drop my head down onto the table. I want to drop the muscles in my face and I just go exhausted.
Instead of going, “Oh, I’m noticing that I’m sad,” be compassionate to your sadness, but bring it straight back to the present, pull your shoulders back. I’m actually just making space for the sadness. I don’t slump and jump into bed and stay there all day. Not that there’s anything wrong with that, but I’m not engaging in sadness. I’m not just responding to sadness with apathy or depression, but I’m actually just spending time there and just going, “Yes, Kimberley, this is sadness. This is the sensation of sadness. It’s okay to have these.” Let’s stay with them. We don’t have to stay with them all day, but let’s just honor them first. Let’s stop jumping to mindfulness and compassion really fast. Let’s actually stay in the sensations. You can still go about your day. You can still be highly functioning. We still want you to be doing those mindfulness and those exercises. But my question to you is: Are you really allowing that to be there or are your emotions holding you hostage? – which I think is what was happening.
As I’ve always said to you, if you have a fear, stare it in the face. That’s how you get empowerment over that fear. If you avoid the fear, that fear has power over you. And then you’re always going to feel like your fear controls your life.
The same goes for sensations. If you have uncomfortable sensations and you immediately remove your attention from them to the present or other things, now your sensations have control over you. You’re giving them all the power and you’re afraid of them.
This is where I pose another question: Are you afraid of your uncomfortable sensations? If so, let’s practice feeling them as an exposure. Without knowing it, my coach who is not an exposure therapist is technically giving us a mini-exposure by saying, “No practice staying in the sensations of sadness or anxiety or happiness or exhaustion or whatever it may be. Practice tolerating and staying with them and still doing what the non-anxious you would do, or the non-sad you would do.”
Like I said, I’m not going to say, “Oh, I have to feel my sadness. I need to stop what I’m doing, stop this podcast and go and lay in bed.” I’m still going to talk to you guys and do what lines up with my values, which is to talk with you guys, connect with you guys, and so forth. But I’m going to say, “Okay, I’m observing that my shoulders feel that heavy feeling or my head feels that heavy feeling or my heart hurts. Can I just breathe into that?”
Now you may want to set some timers for this and say, once you identify it, “Okay, for the next 15 seconds, I’m going to just do this for 15 seconds.” Then you may say, “Okay, let’s try it for 30 seconds.” While I feel this anxiety – shortness of breath, tingling, tight chest, derealization, lump in your throat, panic sensations, racing thoughts – while I tolerate these sensations, can I practice coupling them with my life? So, while I’m feeling the emotion and the sensation, can I type up my email? Can I couple those two together? And when I do that, I might even say to myself, “Okay, this is me doing an email, writing an email while having the sensations of sadness or anxiety or anger or shame or whatever it may be.” Just by that, you’re having this experience of learning how to have emotions and sensations and you’re learning a sense of mastery over them.
Now, some of you have probably thought like, “Well, she’s told me this before,” which is why I said I’m slightly embarrassed because I know this stuff and I’ve probably said it on this podcast before, but I wasn’t practicing it.
Now, humbled to say that we’re all working this out. We’re all figuring this out. I was just listening to this wonderful meditation from my meditation teacher. He was saying that meditation is really like a huge Ashram. If you had the job of cleaning a large Ashram, you’d start in one room and you’d go to the next one, you’d go to the next one, and you’d go to the next one. You’d slowly get it done. By the time you finish, the first room you cleaned is dirty again. So you got to start again.
He’s like, the goal of meditation is not to get the house clean and be like, “Good, I’m done. I’m all done,” slapped my fingers together. “It’s all good.” That’s not what this is about. That’s not what recovery is. I really resonated with that. I feel like I have to tell my clients these stories as well because recovery isn’t a one-and-done. For me, literally, that’s me. I’ve cleaned every room in the house. I’ve circled back. And now I’m like, “Oh, there’s another thing. There’s another area of improvement for me. Oh no. Oops.” You know what I mean? My son always goes, “Oops.” It is total “Oops, okay.” This is a wonderful opportunity for us.
This is not about learning how to be uncomfortable and you’re done. This is about really having mastery over any sensation, any thought, any feeling that you may have. Any urge, any image, anything – having mastery over that. Not even mastery. Let’s just actually scale back. Let’s actually say, “Just knowing you can,” that’s enough. Let’s not talk about mastery. That sounds too big for me right now. Let’s just talk about knowing that I can. If I had to have anger or I had to have sadness or had to have anxiety, I know I could. Let’s stay there.
I hope this has been helpful. I am more than happy to share with you my shortcomings because I think that it makes me very human. It gives you permission to be very human. You guys know that I try not to take myself too seriously. I am on a journey with figuring this out too.
Hey, let’s just keep cleaning one room at a time and enjoy this learning.
Thank you so much for listening. Please do leave a review if you enjoy the show or not. Please leave an honest review. We would love to get a review from you. I’m just sending you much love. Take care, everybody. These are difficult times. I want to really offer my loving-kindness to you, offer a gesture of kindness and warmth and compassion to you if you are struggling.
Have a wonderful day. I will talk to you soon.
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today we have on Christian Newman, the Health Anxiety Coach, to continue our discussion on health anxiety. Christian was on the podcast a while back and because we get so many questions about health anxiety, we decided it would be great to have him on again to answer some of your questions. On this episode, Christian answers “How do I know if my symptoms are anxiety or something else?”, “Is there anything other than CBT and ERP that I can use to treat health anxiety?”, “How do I stop googling my symptoms?”, “How do I stop focusing on sensations?”, and “How do I learn to accept a doctor’s diagnosis?” Christian also shares a bit about his 30 day detox program to help you recover from health anxiety.
 Follow Christian on Instagram @healthanxiety.coach
Follow Christian on Instagram @healthanxiety.coach
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information.
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit podcast. Today, we are going to talk about BFRB’s. Now, a BFRB is body-focused repetitive behavior. Many of you know, I am an Anxiety Specialist; I specialize in OCD and OCD-related disorders. Those related disorders can involve body-focused repetitive behaviors including hair pulling, skin picking, and nail-biting.

Today, I want to give you eight tips to help you manage your BFRB. This is also really helpful if you have any behavior in your life that you want to adjust and change. It is also helpful if you are a family member or a loved one of someone with a BFRB.
The eight tips we are going to discuss today are:
- Identify specifically where you’re engaging in your body-focused repetitive behavior.
- Identify when you engage in your BFRB.
- Identify what emotions trigger your BFRB.
- Identify what thoughts you are having.
- Find alternative behaviors.
- Block the behavior specifically related to the body part.
- Find support.
- Practice self-compassion daily.
Above all else, I want you all to remember that you are not your BFRB. You are way more than this thing that you struggle with. You have so many other beautiful characteristics and strengths and abilities. If you can introduce a self-compassion practice, you will find immense benefit from just gently nurturing the suffering that you are feeling. This is so important for everybody, but particularly for those who are really hard on themselves.
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information.
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today I want to talk to you about a question that recently was asked by one of my awesome Instagram followers. This person asked me "Kimberley, how do I relax and be self-compassionate when I suddenly find myself with extra time on my hands?" This is such a fantastic question and a really timely one as well. So today we are going to discuss the skill of sitting still. Ask yourselves "When was the last time you allowed yourself to sit still?" and "When was the last time you allowed the discomfort you may be feeling to just be there?"
 Maybe you are thinking to yourselves that you have done nothing but sit still since COVID began, but even if this is true when was the last time you sat still and created space for your emotions to rise and fall? When was the last time you allowed yourself to experience your emotions and feelings without judgment? This is key. You may have been sitting still, but you may have been judging yourself at the same time. True restoration begins when you allow those emotions and feelings to be there without judgment. Are you resisting, pushing away, avoiding, or judging? Or are you willingly allowing yourself to feel all of the feelings? Often when we are stressed, we try to busy ourselves. This is usually an attempt to not feel the discomfort. Ask yourself, are my actions effective in the long term? Resisting, avoiding, and distraction may feel helpful in the short term, but is it really effective for the long term? I invite you to slow down and gently and compassionately make space for the present moment. You may not feel an overwhelming sense of calm and that is OK. Your self-compassion is not done to remove your discomfort, it is done to soothe the discomfort. I am asking you to try slowing down. To schedule time to just be still. Allow the discomfort and the quiet. Make space for all of your feelings and emotions as they rise and fall.
Maybe you are thinking to yourselves that you have done nothing but sit still since COVID began, but even if this is true when was the last time you sat still and created space for your emotions to rise and fall? When was the last time you allowed yourself to experience your emotions and feelings without judgment? This is key. You may have been sitting still, but you may have been judging yourself at the same time. True restoration begins when you allow those emotions and feelings to be there without judgment. Are you resisting, pushing away, avoiding, or judging? Or are you willingly allowing yourself to feel all of the feelings? Often when we are stressed, we try to busy ourselves. This is usually an attempt to not feel the discomfort. Ask yourself, are my actions effective in the long term? Resisting, avoiding, and distraction may feel helpful in the short term, but is it really effective for the long term? I invite you to slow down and gently and compassionately make space for the present moment. You may not feel an overwhelming sense of calm and that is OK. Your self-compassion is not done to remove your discomfort, it is done to soothe the discomfort. I am asking you to try slowing down. To schedule time to just be still. Allow the discomfort and the quiet. Make space for all of your feelings and emotions as they rise and fall.
I hope this was helpful and I hope that you remember to be kind and gentle with yourself.
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information.
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today we have on the amazing Joshua Fletcher who some of you may know from Instagram as Anxiety Josh. Joshua is a psychotherapist in the UK as well as someone with lots of lived experience with anxiety disorders. He is here today to talk to us specifically about panic attacks and panic disorder. 
Joshua shares his lived experience with panic, derealization/depersonalization, agoraphobia, and anxiety. He tells about his first panic attack and how that led to multiple panic attacks per day. This led him to planning his days around how to avoid having another panic attack. He shares the importance of psychoeducation for people who are experiencing any kind of anxiety disorder including panic. This is not for reassurance purposes, rather it is important to demystify the experience of anxiety. Once you learn what is happening, the anxiety loses some of it's grip. We know that anxiety thrives in the uncertainty and the unknown so becoming educated on what is happening in your brain and body is really so crucial for recovery. Joshua discusses hypervigilance and how this really is at the heart of anxiety disorders. He gives some tips and tools to help if you have been diagnosed with an anxiety disorder including panic disorder. We end the discussion by talking a bit about self-compassion and how important it is to recovery. I hope you enjoy this conversation as much as I did. Joshua has so much wisdom to share and I think you will find his words not only helpful if you are struggling with an anxiety disorder, but also really inspirational as well.
Instagram @AnxietyJosh
Click here to find links to Joshua's books, podcast, and more!
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information.
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today I want to share with you the 5 mindfulness tips that I use with my clients to help manage symptoms of anxiety and depression.  The first tip is to observe. Instead of taking thoughts as fact, try simply observing your thoughts. An example may be "I am having the thought that bad things may happen." The second tip is to be curious. If you are able to be curious, you can actually change the narrative. Instead of being rigid, try being open to other possibilities. The third tip is to leave judgment behind. We often make the statement that our thoughts and feelings are wrong. Instead leave out the judgment and try "I am noticing this feeling is making me uncomfortable." This brings you back to a place of objectivity. The fourth tip is to be present. Bring your attention back to the present moment. Try to not focus on the past or the future. The fifth and final tip is to catch the stories you tell yourself. Be very careful when you say things such as "I can't handle this." Try to reframe that statement with "I can tolerate the discomfort." or "I can do hard things." I hope these tips have been helpful to you. I know that I find them incredibly helpful and use them often myself and with my own children.
The first tip is to observe. Instead of taking thoughts as fact, try simply observing your thoughts. An example may be "I am having the thought that bad things may happen." The second tip is to be curious. If you are able to be curious, you can actually change the narrative. Instead of being rigid, try being open to other possibilities. The third tip is to leave judgment behind. We often make the statement that our thoughts and feelings are wrong. Instead leave out the judgment and try "I am noticing this feeling is making me uncomfortable." This brings you back to a place of objectivity. The fourth tip is to be present. Bring your attention back to the present moment. Try to not focus on the past or the future. The fifth and final tip is to catch the stories you tell yourself. Be very careful when you say things such as "I can't handle this." Try to reframe that statement with "I can tolerate the discomfort." or "I can do hard things." I hope these tips have been helpful to you. I know that I find them incredibly helpful and use them often myself and with my own children.
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information.
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit. Today we are discussing Exposure and Response Prevention or ERP. So what exactly is ERP? Well, many years ago a psychologist created exposure therapy, which is where we expose people to their fears. If you were afraid of dogs, we would expose you to pictures of dogs and then videos of dogs and then we would probably ask you to go pet a dog, that is exposure therapy.  This was found to be highly successful; however, over the course of time, more research suggested that doing exposures alone is good, but it doesn't completely address the whole picture of OCD because OCD does not just involve obsessions, it also involves compulsions. Exposure therapy did not really address compulsions. So a different method was added on and that is the response prevention. You expose yourself to your fear and then you would do response prevention, which would mean you would not engage in the compulsion to remove the discomfort, uncertainty, or anxiety that you are feeling.
This was found to be highly successful; however, over the course of time, more research suggested that doing exposures alone is good, but it doesn't completely address the whole picture of OCD because OCD does not just involve obsessions, it also involves compulsions. Exposure therapy did not really address compulsions. So a different method was added on and that is the response prevention. You expose yourself to your fear and then you would do response prevention, which would mean you would not engage in the compulsion to remove the discomfort, uncertainty, or anxiety that you are feeling.
ERP is a treatment that addresses both the obsession by exposing and the compulsion by doing response prevention. Now, this is groundbreaking and the research has shown that the outcomes are really good, which is wonderful because for many years, we did not have a great treatment for OCD. Since then we have actually added on other modalities to make it even better. We have inhibitory learning, acceptance and commitment therapy, compassion focused therapy, and mindfulness-based cognitive behavioral therapy. All of these additional modalities really help to increase motivation and help to manage your discomfort as it rises and falls.
A lot of people will ask if ERP can work if you do not engage in physical compulsions because as we know many people with OCD will engage in hidden compulsions that no one can see. Those are typically avoidance and mental compulsions. From the outside you may never know that they are struggling with mental compulsions all day because they are ruminating and playing out potential scenarios in their minds. It is so important to identify the mental or avoidant compulsions you are doing and that would be a part of your ERP as well.
So that's ERP in a nutshell. Is it easy? Oh no, it's not easy. Is it hard? Oh yes, it is hard. But what am I about to say, say it with me everybody, it is a beautiful day to do hard things. Can you do hard things? Absolutely.
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information. Beginning today March 19th and continuing until April 1st, ERP School will be available with bonus material. This will be an amazing training on the motivational skills Kimberley teaches her clients to help them in their treatment and recovery!
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today we are so lucky to have Dr. Jonathan Grayson on with us again. Dr. Grayson is a psychologist who has been specializing in the treatment of OCD for more than 40 years. He is also the author of Freedom from Obsessive-Compulsive Disorder and founder of The Grayson LA Treatment Center for Anxiety and OCD. He is here today to talk to us about magical thinking. I am actually getting asked a lot recently about magical thinking. People have a lot of questions about what it is and how it relates to OCD and anxiety. 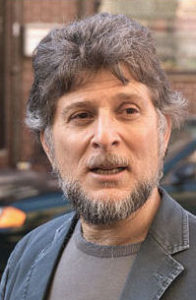 Dr. Grayson starts off by giving us his definition of magical thinking. He explains that magical thinking is really on a continuum. On one end you may have a person without OCD who engages in minor superstitions and on the far end you may have a person with OCD who has magical thinking that is actually interfering in their daily life. He says that most of the time with OCD, the magical thinking does not seem to have an obvious connection between the fear and the ritual.
Dr. Grayson starts off by giving us his definition of magical thinking. He explains that magical thinking is really on a continuum. On one end you may have a person without OCD who engages in minor superstitions and on the far end you may have a person with OCD who has magical thinking that is actually interfering in their daily life. He says that most of the time with OCD, the magical thinking does not seem to have an obvious connection between the fear and the ritual.
Dr. Grayson spends a good amount of time discussing magical thinking in the context of spiritual and religious beliefs as well as how magical thinking relates to scrupulosity. He also shares his thoughts on scapegoating as a form of magical thinking. He shares with us a bit about how someone can get better and overcome magical thinking. He says that this is really just about taking the risk of uncertainty similar to all OCD treatment. He says you should ask yourself "Is this magical thinking actually working? Is it bringing you any peace?" This episode is full of such wisdom. I learned a lot myself and I hope you all will find it helpful.
Dr. Grayson's book, Freedom from OCD, is now out as an audiobook! Click here for more information.
The Grayson LA Treatment Center for Anxiety & OCD
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information. Beginning today March 19th and continuing until April 1st, ERP School will be available with bonus material. This will be an amazing training on the motivational skills Kimberley teaches her clients to help them in their treatment and recovery!
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Welcome back to another episode of Your Anxiety Toolkit Podcast. We have a lot to tackle in this episode! We are going to be talking about a really important topic which has a lot of confusion surrounding it. Today we are going to explore the difference between an intrusive thought and a mental compulsion.
OCD starts with an obsession. This is an intrusive, repetitive, unwanted thought, feeling, sensation or urge that you cannot control this. Once you've had that intrusive thought, feeling, sensation and urge, you usually feel anxious and uncomfortable because it is unwanted. You then have this natural instinct to try and remove the discomfort and the uncertainty that you feel. This is what we call a compulsion. Usually we feel some form of relief from the compulsion, but this becomes a problem because it only reinforces to our brain that the thought was important. Your brain continues to send out the alarm that the thought must mean something. Now many of us are aware of the form that physical compulsions can take such as hand-washing, jumping over cracks, moving objects and so forth. Actually one of the most common compulsions is mental and that takes the form of rumination. The problem people run into is that rumination is sometimes hard to identify. That is why I am doing this episode because so many people have asked, how do I differentiate between the intrusive thought and a mental compulsion? And what do I do? We know we should not be blocking thoughts, so how do we stop mental compulsions. If I'm not supposed to suppress my thoughts, what am I supposed to do if I catch myself doing mental compulsions? Is stopping mental compulsions thought suppression?"
I would say, technically, no. But it depends. Let's go straight to the solution. We want to acknowledge that we're having an intrusive thought, feeling, sensation or urge or an image. our job is to do nothing about it. We need to do our best not to solve that uncertainty or remove ourselves from that discomfort. That's our goal. And then our job is to reintegrate ourselves back into a behavior that we were doing, or we would be doing, had we not had this thought. So here is an example. Let's say I'm typing. I have an intrusive thought about whether I'm going to harm my child. So I have this, I'm going to acknowledge that it's there. I'm actually going to practice not trying to make that thought go away. But instead, bring that sensation or thought with me while I type on my computer. As I'm typing, I'm going to notice the sensations of my fingertips on the keyboard. I'm going to notice the smell of the office. I'm going to notice the temperature of the room I'm in. And I'm going to then catch if my mind directs away from this activity towards trying to solve. If I catch myself trying to solve it then I am going to bring my attention back to what I'm doing. I find that if I'm getting caught in some kind of mental rumination, I get down on the ground and I start playing with my son. The OCD may continue to try and get your attention, but you are going to continue with what you are doing and not engage with the thoughts. It is important to remember that compulsions feed you back into a cycle where you will have more obsessions, which will feed you back into having more compulsion's. It's a cycle. We call it the Obsessive Compulsive Cycle. So we really want to sort of be skilled in our ability to identify the difference. This is really, really hard work. I think about when you're originally first learning anything, everything is really confusing and everything looks kind of the same. When you first start doing it, these are going to look very similar and it's going to be difficult to differentiate the difference, but once you get better at being around this and labeling it and catching it, you will be able to see the differences in these two things, even if it's very, very nuanced or they look very, very similar.
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information. Coming in March 19th ERP School will be available with bonus material!
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Coming March 15th, we are offering our free training, The 10 Things You Absolutely Need to Know About OCD.
Transcript of Ep. 180
This is Your Anxiety Toolkit episode number 180.
Welcome to Your Anxiety Toolkit. I'm your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn't get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big fat virtual hug, because experiencing anxiety ain't easy. If that sounds good to you, let's go.
Welcome back, everybody. Hello. Thank you for being here with me. We have a lot to tackle in this episode, so I am going to jump in as quick as I can. I know this is such a huge concept and topic, and there's so much confusion around it. So let's really today talk about the difference between an intrusive thought and a mental compulsion. We also want to figure out which ones we want to work with and which ones we want to allow. We want to talk about the difference between allowing a thought and engaging in a thought. There's so much to cover here. So before we get started, a couple of really exciting things, I really want you to keep an eye out for. On March 15, 2021, we are relaunching the free OCD training. It's called the 10 Things You Absolutely Need to Know About OCD.
It's not called the 10 things you need to know. It's called the 10 Things You Absolutely Need to Know About OCD. I have shared this free training multiple times, tens of thousands of people have taken this training. I've gotten nothing but amazing responses back. And the coolest thing is people even said, "I've watched it before. This is the second or third time I've watched it when you released it. And it really reminded me of these core concepts that we have to remember when we're talking about OCD." So even if you've watched it before, even if you're pretty well versed in OCD, I still encourage you to listen and take the free training. It's just jam packed with information and science and all the good stuff. And even if you're a therapist, I encourage you to take it. So if you're interested, go over to cbtschool.com/10things, or you can click the link in the show notes.
I am so excited to share that with you. Now, one more thing, keep an eye out, because as of March 19th, we are relaunching ERP School with some exciting bonuses, which I will announce in next week's episode. So excited again to share this with you. And what an amazing community, what an amazing opportunity I've had to teach so many people about ERP. And now also teaching therapists. We have now got ERP School approved by The National Association of Social Workers. So if therapists out there, you can actually get CEUs for taking ERP School, which is very, very cool. All right, let's get straight to the show. Let's talk about the difference between an intrusive thought and a mental compulsion first. So the first important piece to remember here, as we pull apart what to do with what thoughts, because that's really what this is about.
We must first understand the foundation of OCD. So OCD starts with an obsession. This is an intrusive, repetitive, unwanted thought, feeling, sensation or urge. It's not just a thought. It could be a sensation. It could be a feeling like de-realization or guilt. It could be a sensation like a feeling in your left finger or feeling in your nose or whatever that may be, everybody's different. But it does start with this intrusive thought. And the thing you must remember here is you cannot control this. This is the first experience of OCD, right? You have the intrusive thought, feeling, sensation or urge, and this is the thing you can't control. So there's a really big point right off the bat. The second piece here is once you've had that intrusive thought, feeling, sensation and urge, you usually feel anxious and uncomfortable and it's unwanted. And so your natural instinct is to do something to remove it.
You'll do it to remove the physical discomfort, the emotional discomfort, the uncertainty that you feel. And that is what we call a compulsion. Now, as many of you know, we know the kind of more mainstream compulsions that are known in our society. Hand-washing, jumping over cracks, moving objects and so forth. But one of the most common compulsions is mental. It's thinking. It's rumination. And that's the thing that's really hard to catch. And that's why I'm doing this episode because so many people have asked, how do I differentiate between that intrusive thought and a mental compulsion? And what do I do? Like I said at the beginning, I'm not supposed to block thoughts, but I'm not supposed to do mental compulsions. And that's thinking too, and what this does, right? So let's go back to the cycle. You have a thought, feeling, sensation and urge.
It makes you uncomfortable. Then you do a compulsion to make it go away. And usually you do get some form of relief. But the problem with this is that then it reinforces that that thought was important. Therefore, your brain continues to send out the fire alarm, the safety alarm, the smoke detector, it sets off all of those alarms in your brain and then sends out more anxiety with more of that thought, feeling, sensation and urge. So let's go back to the main concept. You're not to try and suppress your thoughts because the more that you suppress your intrusive thoughts, the more you have them. I've done full episodes about this in the past. So if you want to go back and listen, suppressing your thoughts will only make them worse. But here is where it gets tricky. People will say again, "If I'm not supposed to suppress my thoughts, what am I supposed to do if I catch myself doing mental compulsions? Is stopping mental compulsion's thought suppression?"
And this is where I would say, technically, no. But it depends. So what we want to do, let's go straight to the solution. We want to acknowledge that we're having an intrusive thought, feeling, sensation or urge or an image, right? It could be an image too. And then our job is to do nothing about it. To do our best not to solve that uncertainty or remove ourselves from that discomfort. That's our goal. And then our job is to reintegrate ourselves back into a behavior that we were doing, or we would be doing, had we not had this thought. So let's say I'm typing. I have an intrusive thought about whether I'm going to harm my child, or I have an intrusive thought about whether I cheated on my partner, or I had an intrusive thought on whether I'm gay or straight, or I had an intrusive thought about harming somebody, or a religious obsession, or a sensation, or a health anxiety sensation.
So I have this, I'm going to acknowledge that it's there. I'm actually going to practice not trying to make that thought go away. But instead, bring that sensation or thought with me while I type on my computer. As I'm typing, I'm going to notice the sensations of my fingertips on the keyboard. I'm going to notice the smell of the office. I'm going to notice the temperature of the room I'm in. And I'm going to then catch if my mind directs away from this activity towards trying to solve. If I catch myself trying to solve, yes, I am going to practice not doing that thinking. I'm going to practice not trying to solve it. And then bring my attention back to what I'm doing. I find that if I'm getting caught in some kind of mental rumination, I get down on the ground and I start playing with my son.
He's really into Lego right now. And so I fully, fully throw myself into this. I do my best to fully engage as best as I can. Now, I'm still going to have the presence of intrusive thoughts because I cannot control that. So it's going to sound a little bit like this. OCD is going to say, "Hey, what about this? What if this happens?" And I'm going to say, "Hi, thought. I'm actually typing an email right now. And that's what I'm going to do. You can be there. I'm going to allow this uncertainty to be here and I'm going to keep typing." So then I start typing. And then OCD will be like, if I were to externalize it, would be to say, "No, no, no, no. This is really important. You really have to figure this out."
And I'll go, "No, thank you. I'm really cool that you're here, but I'm going to type." And then it's going to say, "Hey, Kimberley, this is really important. And if you don't give me your attention, I'm going to... Something really bad is going to happen." And I'm going to go, "Thank you. But I'm writing an email right now." And then you're going to be like, wow, I'm doing pretty good. Look at me go. I'm fully practicing the skill of not engaging in my intrusive thought. And then it's going to say, "Listen..." Let's say I'm impersonating OCD. It's going to say, "Listen, I am not going to stop bugging you until you give me your attention." And I'm going to go, "That's fine. I'm actually going to call your bluff on that. I'm writing this email. You do not get to tell me what to do." And it's not going to give up.
It's going to keep going. "Kimberley, Kimberley, Kimberley, Kimberley, you must pay attention to my thoughts. You must pay attention. I'm trying to alert you to a very big danger." And often this is where people get worn down. They're like, "Oh my gosh, it's not going away. Maybe it is right. Maybe I should do it. Maybe I can't handle this anxiety. Maybe this is too much for me. Maybe it's just easier to do the compulsion." But I'm going to be here with you, urging you to keep allowing that intrusive thought to be there. It will basically roll over and start crying and fall asleep at some point, like a toddler, who's too tired and is rejecting his nap. But all he needs is to nap. It eventually will die down, but you have to be willing to stick and be consistent with not engaging in the pleads of OCD, the urgency of the obsession, the catastrophization of the obsession.
Because it's going to be making it into a... What do they say? A molehill into a mountain. It's going to be making a small problem, a big problem. And what I mean by that is the present of a thought is not dangerous. It doesn't mean it's a fact. It doesn't mean it requires your attention. Some people with OCD have a part of your brain that's going to set this thought on repeat. And because we've tried to suppress it in the past, it is probably going to want to be very, very repetitive. And your job is to do nothing at all. If you do, and I'll say this again, if you do catch yourself doing mental compulsion's, it's okay to stop doing that. That's not thought suppression. As long as you're... You don't want to over-correct. So if you catch yourself doing mental compulsions, don't over-correct by also trying to block the thought.
That's where we get into trouble. Instead, you just do a small correction back to what am I doing? What am I engaging in right now? What do I value? Because we do not value compulsion's. Compulsion's feed you back into a cycle where you will have more obsessions, which will feed you back into having more compulsion's. It's a cycle. We call it the Obsessive Compulsive Cycle. So we really want to sort of be skilled in our ability to identify the difference. If you can't identify the difference it's going to be really hard to know which is which, and how to respond in those moments. And a lot of this is when we're super anxious, it's really hard to think logically. It's really hard to think... Is this true or is it not? Or so forth. It's not even helpful in that moment.
Whereas, it may be like three days later. You're like, "Oh my goodness, what was I thinking? That was a bit strange. I wonder why I got so caught up in that." And that's because when we're anxious, our brain has a difficult time coming up with problem solving that is effective. So the more you can be able to identify it, and I encourage my clients throughout the day is catch yourself doing mental compulsion. Don't beat yourself up, but practice this idea of going, "This is me doing a mental compulsion. This is me having an intrusive thought. This is me having an intrusive thought and wanting to do mental compulsion." And being able to label them so that in the moment when you really are at a nine or a 10 out of 10 of anxiety, or uncertainty, or discomfort, you're able to be more skilled in your response.
Super, super, super important stuff here, guys. But we don't want to shame here. Again, this is really, really hard work. I think about when you're originally first learning anything, everything is really confusing and everything looks kind of the same. I always think of like The Devil Wears Prada, this is a crazy example, but the actress is laughing at these people because they're looking at a belt that looks almost the same, but it's very different in their eyes. And the one main character is like, "They're the same belt." And they look at her like she's crazy. And this is the same, right? When you first start doing it, these are going to look very similar and it's going to be difficult to differentiate the difference. But once you get better at being around this and labeling it and catching it, you will be able to see the differences in these two things, even if it's very, very nuanced or they look very, very similar.
Okay, that's all I'm going to say for now. The tools are the same. If you really want to go back and practice and learn these mindfulness skills you can practice, go back and listen to some of the previous podcast episodes. I actually encourage you to go back and listen to some of the earlier episodes, because in those episodes, I totally, I was laying out this awesome content on how to be mindful. Some of my best podcasts are the very first few ones, which is like back-to-back major skills, major tools. It was laying the foundation for how to be mindful with obsessive thoughts. So go back and listen to those or sign up for the free training coming up or, and you can also sign up for ERP School, which is coming back very, very soon.
We also have Mindfulness School for OCD, which is a course that really deep dives into practicing mindfulness related to obsessions and compulsions. So that's there for you as well. Okay. A lot. Sorry, I'm talking so fast. It's something I'm so passionate about and is something that I really wanted to make sure I covered and get very clear on. I've had a couple of you reach out and really be stressed about figuring out the difference. I'm hoping that's super helpful.
One last thing before we go, please do leave a review. I know I keep begging you at the end of every episode, but it really would mean the world to me. If you get anything from the podcast and you want to give back in any way, I would love a review from you. Your honest review, you don't have to fabricate anything. I really love them. I read every single one. And once we get to 1,000 reviews, we will give away a free pair of Beats headphones so that you can hear me crystal clear in your ears. And you of course can pick the color of your choice with those. So all my love to you.
Please do go and leave a review. I hope today's episode [crosstalk 00:17:05] was helpful. And get excited [crosstalk 00:17:05]. All right, have a good one, guys. All my love to you. It is a beautiful day to do the most beautifully difficult hard things.
Please note that this podcast or any of the resources from the CBTschool.com should not replace professional mental healthcare. If you feel you would benefit, please reach out to a provider in your area. Have a wonderful day. And thank you for supporting CBTschool.com.
Welcome back to another episode of Your Anxiety Toolkit Podcast. Today I want to focus a bit on OCD treatment. I want to share with you all 8 tips that I think will really help to fast-track your OCD treatment. The first tip is to get support. 
That may people from people in your life or it may be from social media, organizations in the OCD community, or online support groups. The second tip is to pace yourself. Find a pace that works well for you, not too fast, not too slow. The third tip is to give yourself time to feel all the feelings about your OCD treatment. You are likely going to ride a wave of emotions and that is OK. The fourth tip is to stop judging yourself for your obsessions and compulsions. Being critical of yourself on serves to get in the way of your recovery. So go easy on yourself. The fifth tip is to embrace uncertainty. Learning to live with uncertainty is key to recovery in OCD treatment. The sixth tip is to stare your fear in the face everyday. Remember when we turn away from our fear, OCD only becomes stronger. The key is to do those hard things. The seventh tip is to find your motivation. What is your motivation for wanting to get better? The eight and final tip is understanding and accepting that you cannot control your thoughts. The only thing you can control is your reaction to those thoughts. I hope these tips will help as you progress through your OCD treatment. If I can leave you with just one thought that would be "It's a beautiful day to do hard things."
If you get a moment, please go over to wherever you listen to podcasts, whether that be Apple Podcast, Stitcher, Spotify, Podbean, and leave an honest review. Tell me how you feel about it, whether it's helping you, what you'd like to see. We are going to give away a pair of Beats headphones of your choice of color once we hit a thousand reviews!
ERP School, BFRB School and Mindfulness School for OCD are open for purchase. Click here for more information. Coming in March 19th ERP School will be available with bonus material!
Additional exciting news! ERP School is now CEU approved which means that it is an accredited course for therapists and mental health professionals to take towards their continuing education credit hours. Please click here for more information.
Coming March 15th, we are offering our free training, The 10 Things You Absolutely Need to Know About OCD.
Transcript of Ep. 179
This is Your Anxiety Toolkit - Episode 179.
Welcome to Your Anxiety Toolkit. I’m your host, Kimberley Quinlan. This podcast is fueled by three main goals. The first goal is to provide you with some extra tools to help you manage your anxiety. Second goal, to inspire you. Anxiety doesn’t get to decide how you live your life. And number three, and I leave the best for last, is to provide you with one big, fat virtual hug, because experiencing anxiety ain’t easy. If that sounds good to you, let’s go.
Welcome back, my friends. Hello, Happy Friday. This is when it’s released. If you’re not listening to this on a Friday, Happy whatever day you’re listening, Happy Day.
How are you? Take a breath. Where are you? What are you doing? What do you see? What do you smell? It’s a beautiful day.
Thank you for being here with me. It is a beautiful day to do hard things, as always. But today, we’re actually talking about exactly that, talking about how to do really hard things in the form of talking about the eight things you can do to fast-track your recovery. It could be OCD recovery, it could be health anxiety, panic disorder, eating disorder, whatever it may be. But we’re probably going to put a focus today on OCD, mainly because I am getting ready. This is very exciting.
Let me go off on a tangent. I’m getting ready to relaunch the free training that we offer twice a year called The 10 Things You Absolutely Need to Know about OCD. It’s a free training. We’ve offered it now for almost three years, and I offer it twice a year over... not over a thousand, over tens of thousands of people have watched this training. It’s quite amazing. So many people have given me amazing feedback on it. A lot of people have said that this was their first introduction to OCD and the education to OCD. I’m just so happy to share this with you.
We will be releasing this training again on March 15, so get ready. I will send you all the details when we get there, but for right now, you could just get really excited and you can listen to this episode, which is really again, talking about not the basics of OCD, even though a lot of people who’ve taken that free training said they go back every time I launch it and rewatch it because it’s a really great reboot on these major basic concepts. Today, we’re going to talk about bigger concepts, like really looking at treatment and how to fast-track it. So, let’s get started.
Before we start, actually, again, I’m going to ask you for a favor, if you would have a moment and you feel so inclined, please go and leave a review. I am on a massive... What would you call it? Effort to get more reviews, not because I need the ego stroke at all, but because I have been told by multiple business people that if you want to help more people and get this free resource out to more people, you do have to have a ton of reviews. The more reviews you have, the more likely people are to click on the podcast and try it. My goal is to create really, really good content, but they have to actually click the content to get helped by the content. So if you could help me with that, that would be amazing.
I have offered an incentive. We are having an exciting challenge where we’re challenging ourselves to get a thousand reviews. Once we get a thousand reviews, I’ll be giving away a pair of Beats headphones to one of the lucky reviewers of your color choice as a thank you. So, that’s there. I would love to have you write a review. All right, let’s get into the show.
We’re talking about the eight tips to fast-track your OCD treatment.
- Get support.
This was actually the #8 point, but I actually brought it up to #1. If you are willing to do hard things, which you will because OCD treatment requires you to do many hard things, you will need support. Now I know what you’re probably thinking. “I don’t know anybody who has OCD,” or “I don’t have enough money for treatment,” or “I don’t know who to ask.” And that’s why this podcast is here. This is a free service to help you feel supported. And if listening to this podcast is your form of support, well, I am so, so grateful and blessed to have that opportunity. But even better than that is to get support by people who are in a similar situation and it does not have to cost you money. It does not have to cost you time.
The use of getting support for OCD might look like social media accounts. There are so many advocates on social media, Instagram, Facebook. This is a really wonderful way to get support. You might go to OCD Gamechangers or the International OCD Foundation, where they have programs and free town hall and fireside chats where you can feel supported because you’re in an area of like-minded people. You might join a support group. There are many GOALS support groups. It’s G-O-A-L-S support group. If you Google it, there are many around the country of the United States where they’re free support groups for people. They are online forums. I have a free Facebook group called CBT School Campus, which is a group of the most kind of supportive people who are also on their journey.
So, get support. You can’t do hard things on your own all the time. You can do them on your own some of the time, but it fast-tracks it if you really do have support and people cheering you on.
The other thing to remember is you don’t have to know someone who has OCD. Find somebody who’s also doing something difficult and say, “Hey, I’m doing a hard thing. You’re doing a different hard thing, but I wonder if we could support each other.” Most of the time, people are so relieved not to do hard things on their own. So, get support.
- Pace yourself.
When you want to fast-track your treatment and your recovery, your instinct is to go in great guns. In Australia, we call it great guns. Great guns is full-on going in, giving it your biggest effort. And that’s good. Great guns is awesome, but you have to pace yourself. You can’t sprint a marathon. You’ll get into the first mile and you’ll collapse. This is about pacing yourself and having a clear plan.
One of the biggest areas I make as a clinician is when I create a treatment plan for my patient or my client, and it’s not a good pace. It’s not a good beat. You can hear me clicking. You can’t go really fast and then taper out. You lose momentum. So what you want to do is pace yourself at a cadence that feels really right and is doable and is realistic, that you can make a part of your daily life because it’s not realistic to do four hours today and then zero hours tomorrow, and then two hours the next day. Try and find something that you can do a little bit every day.
- Give yourself time to be mad, sad, sad, resentful, and have whatever feelings you have about this OCD treatment or this recovery process.
You’re going to have lots of emotions and you have to prepare yourself for that. You have to be willing to ride the many emotional waves of recovery. It’s not just a matter of sitting down and doing exposures and going on about your life. You are going to have to feel all kinds of emotions, and that can be really overwhelming and painful. So give yourself time to have those emotions.
- Stop judging yourself for your obsessions and your compulsions.
One of the things that is the most demotivating actions we can do is criticize ourselves for where we’re at. This is a podcast episode about fast tracking. This means what slows us down, looking at what are the things that slow us down so that we can go at the fastest pace possible that is healthy and realistic. And that involves not being critical. Being critical literally does nothing good. It slows you down. It de-motivates you. It disempowers you. It makes you feel more secondary emotions. It does no good.
I know you know that, but sometimes we have to remind ourselves that in the moment, when we catch ourselves judging ourselves for the thoughts or feelings we’re having or judging ourselves for the compulsion we’re doing is to go, “Wait, that’s not helping. That’s not effective. That doesn’t get me closer to the goal.” Even if I feel that way and it feels true, I am going to catch this and step out because it’s not effective.
- Uncertainty is key.
If you are not being uncertain, you are taking a detour. Think of it like you’re on a road and you’ve got a destination and you’re getting there. Every time you go off the road, let’s say, you’re going from A to B, going off the road, going towards C is the equivalent of going to certainty. You want to get off the road of certainty and get back on the road to being uncertain. And you will naturally, oops. Whoops, it’s easy. As we took a little detour back into certainty land, turn around, do a U-turn, come on back to the road of uncertainty. That is the fastest route to your recovery. Then you’ve got like a GPS. Over the GPS if you had one in your car, it would be like, “Please do a U-turn. You have taken the wrong route. You are on the road of certainty. Turn around and proceed to the road of uncertainty.” That’s how I imagine the GPS lady or man speaking to you when you’ve gone down that wrong road.
Again, when you catch yourself, don’t beat yourself up. The GPS doesn’t go, “Bad you. You’re a bad person for going on a detour.” She just goes, “Would you please do a U-turn and proceed to the route?”
- Stare your fear in the face every day, learn to play this game, and it is a gap.
This is talking about a Reid Wilson approach who I adore. Reid Wilson’s approach is, this is a game. Your job is to accumulate points. Every time you stare fear in the face, you accumulate points. And we want more points. We want to take the points away from OCD.
I’ll often say to my patients and clients, “I want you to accumulate a hundred points a day.” Let’s say if touching... my bike’s right in front of me. So I’ll say, let’s say touching the handlebar of my bike is a 5 out of 10. If I do that, I get five points. Good job. I’ve only got 95 more to get today. If letting myself have certain thoughts, if that’s a 9 out of 10. Okay, great. Now I’ve got 14 points. I’m getting there. I’m getting closer to my goal. You could say 50 points. If you wanted to start early or easier, you could go to 10 points to start with. That’s fine. But learn to stare your fear in the face every day and play the game. We don’t want OCD getting and accumulating and racking up all the points because they win. Because when we avoid, OCD gets points. We want to try and prevent OCD from hitting its 10, a 100 mark every day. We want to be like, “Nope, I’m going to win this game today.”
- Treatment requires motivation and fast-tracking requires motivation.
Your job is to identify what will happen if you don’t play this game and stare fear in the face. Identify what OCD has taken away from you. PS, little teaser. Next week’s episode is all about motivation. If you struggle with this, we’re going to deep dive into motivation. It’s something that I have been asked about so much lately. So I, of course, scheduled to talk to you about it.
Again, the motivation, it does require a ton. If you want to fast-track your treatment, it does require that you get your wheels moving and you don’t slow down. And that will require keeping in your mind’s eye right in the front. Like, I’m doing this hard work because if I don’t, OCD will take A, B and C from me.
Now, little side note, and we’ll discuss this next week. If that feels a little like pressure or shaming or guilt-tripping on you, we can learn to shift the language around that. Your job again is to try not to judge yourself for what it has taken from you in the past. That’s a really important piece here. But again, I’ll pause there because we’ll go through that next week.
Drum roll... The final major thing that you have to remember to fast-track your treatment, and I did originally have this as #1, but I’m going to finish with it because it’s probably the most important.
- Your recovery requires a deep understanding and acceptance of the fact that you cannot control your thoughts.
Most people, by the time they come to me, have wasted so much time and so much of their life in a wrestle, trying to control their thoughts. No judgment there. That is the natural inclination of a human being. But you have to really drop down and recognize that trying to control, which thoughts come in and out of your mind, is a lose-lose for everybody. The only thing you can control is how you respond to your thoughts. Massive, massive point. That is one of the points we do cover in The 10 Things You Absolutely Need to Know about OCD training, but I really wanted to bring it up again because it’s so important. Everyone gets caught in this one. So it’s just a matter of catching it and going, “All right, I’m in a wrestle with my thoughts. I know I can’t control my thoughts. So I’m going to have to try something different.” The only thing you can do differently is to change how you respond.
The answer to that, let me give it to you, is just to do something different. It’s basically to go, “Oh, this is too big. I can’t solve this. It’s unsolvable. I’m just going to walk away.” It’s sort of like, sometimes my son’s doing a Lego and he’s getting really frustrated because he just can’t seem to figure out this next step and he’s getting more upset and he’s getting more upset. Now he’s sort of ripping at it and pushing out it and things are suddenly breaking apart. I’ll say, “Whoa, this isn’t working step away. Let’s go do something else. We’ll come back later.” That’s really important.
I love you guys. That is the eight tips I have for you to fast-track your OCD treatment. If some of that went too fast and too much, get ready, we’ll do the free training here very soon. I strongly encourage everybody to take it, even if you’ve taken it again, because I’ve added a bonus point this time. Really now it’s 11 things you have to know, but you’ll see that when we get there.
All right. I love you so much. Have a wonderful day. It is a beautiful day to do one hard thing. Whether you choose the hard thing or it’s naturally happening, that’s okay. Just do the hard thing. Be in the hard thing. Give yourself permission for things not to be right and perfect.
Okay, I love you. Have a wonderful day and thank you for listening.
Please note that this podcast or any other resources from cbtschool.com should not replace professional mental health care. If you feel you would benefit, please reach out to a provider in your area.
Have a wonderful day, and thank you for supporting cbtschool.com.